There is a critical mass of evidence supporting the use of cone-beam CT (CBCT) for periodontitis management and periodontal-orthodontic therapy for skeletally mature patients, but there are still too few studies to issue definitive practice guidelines, according to new Best Evidence Consensus (BEC) statements from the American Academy of Periodontology (AAP).
George Mandelaris, DDS, co-chair of the academy's BEC meeting on CBCT, told DrBicuspid.com that broad clinical guidelines that affect an entire profession must be evidence-based, and, right now, there are not enough qualified studies to make such statements possible.
"However, the evidence is mounting and imaging technology is transforming how we diagnose, prognose, and execute for patients," Dr. Mandelaris stated. "Periodontists and general dentists should embrace imaging technology but must not allow it to usurp biology and wound healing principles of surgery nor undermine the value of the team approach to patient care."
The academy published its series of statements in the Journal of Periodontology on September 28.
Periodontal-orthodontic treatment
To address evolving issues in periodontal practice, the AAP convened a panel of experts with knowledge of and experience using CBCT in a range of clinical scenarios. The panel completed a systematic literature review on the scenarios and debated the merits of published data and experiential information. These best-evidence statements provide a clinical bottom line based on the best evidence available, according to the academy.
The series of statements included a summary article and individual statements on periodontal-orthodontic treatment, implant placement, and the management of periodontitis. The statement on implant placement will be included in a separate article.
For the question concerning the use of CBCT in periodontal-orthodontic treatment, the expert panel performed a literature search and found 13 applicable studies. Between panelists' discussion and an analysis of the studies, the panel found that the evidence came from observational studies of low methodologic quality.
"There is limited current evidence to support specific applications of CBCT as a routine part of periodontal-orthodontic treatment," the expert panel concluded.
The panelists, however, did note that CBCT might be useful as a routine part of periodontal-orthodontic treatment in some circumstances:
- When the orthodontic patient is skeletally mature and presents with a malocclusion requiring fixed orthodontic appliances for decompensation
- When the orthodontic patient has a thin dentoalveolar phenotype and dentoalveolar bone deficiencies are suspected
- When the malocclusion patient requires advanced tooth movement and there is increased risk for positioning the roots outside of the orthodontic boundary conditions
- When the orthodontic patient is skeletally immature and requires an interdisciplinary approach to treatment
Periodontal disease treatment
When considering if this imaging system adds clinical value when treating periodontitis, the expert panel winnowed an initial list of almost 900 studies down to 12. It concluded there was little evidence to support CBCT as a routine replacement or even as an adjunct to 2D imaging.
"Current evidence supports the use of 2D full-mouth radiographic series in addition to clinical probing parameters as the gold standards for comprehensively evaluating periodontal structures," the panel wrote.
But again, the experts did note some circumstances in which CBCT might be useful as a routine part of treatment for these patients:
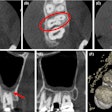
- When an advanced furcation lesion has been detected and dental implants are being considered as an alternative treatment option
- When advanced bone loss has encroached on anatomic structures, such as sinus cavities or the inferior alveolar nerve
- When there is a questionable root fracture, root resorption, or periodontal-endodontic lesion present that could not be identified by 2D imaging and/or clinical evaluation
Dr. Mandelaris noted that this was another example of a lack of evidence for the routine use of CBCT to be recommended.
"3D [imaging] usually provides more useful data," he wrote. "[But] the current studies we evaluated did not suggest that advanced imaging impacts the management of periodontitis alone beyond that achieved with good-quality diagnostic radiographs."
However, this does not mean CBCT cannot help in treatment planning for patients with advanced forms of periodontal disease, Dr. Mandelaris added.
"Because advanced forms of periodontitis often require implant therapy or an interdisciplinary approach at management, CBCT should be considered on a case-by-case basis for more ideal comprehensive care," he stated.
Up to the treating dentist
In the reality of treatment today, there are very few treatment situations in which 2D imaging is the more appropriate imaging option, according to Dr. Manelaris. However, the decision of which imaging system to use must be made by the treating dentist.
"The treating clinician must determine which modality of imaging best suits the needs of the patient for proper diagnosis, treatment outcomes, and safety," he stated.
Disclosures
The American Academy of Periodontology Best Evidence Consensus meeting on cone-beam computed tomography was sponsored by Carestream Dental. No fee was paid to DrBicuspid.com for editorial coverage.