Volumetric changes in radiolucency on cone-beam computed tomography (CBCT) scans may help foretell how effective root canals were in treating apical periodontitis. The study was published on May 11 in the Journal of Dentistry.
A year after endodontic treatment, reversal of the radiographic healing tendency was rare when there was a 20% or more change in radiolucency volume on the scans, the authors wrote.
"The efficacy of root canal treatment for apical periodontitis was predictable," wrote the authors, led by Dr. Ming-Ming Zhang of the Peking University School and Hospital of Stomatology in China.
Predicting the prognosis of a tooth as early as possible is critical for clinical decision-making. Knowing the time frame for radiographic healing of apical periodontitis can assist clinicians in determining whether a root-filled tooth with a periapical lesion can be left alone or needs retreatment.
Until now, there has been little published research that has reported the period of healing after primary root canal treatment, according to the study. In this retrospective study, 162 single-root teeth from 130 patients with chronic periapical periodontitis who had undergone primary root canal treatment were evaluated. Follow-up visits were scheduled at one, two, and four years after the treatment.
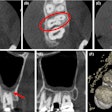
The volume of radiolucency was measured before treatment and during each follow-up visit. Radiographic outcomes were classified as absence, reduction, uncertain, or enlargement. A change in radiolucency volume was considered a reduction or enlargement if it was 20% or more, they wrote.
During the four-year follow-up period, 128 teeth were reviewed at least once, including three that were extracted. Of the remaining 125 teeth, 116 (90.6%) showed a reduction in radiolucency volume, five were uncertain, and four had an increase in radiolucency volume over the one to four years after treatment.
Among the 43 teeth with reduced radiolucency at the one-year mark, 42 (97.7%) continued to show reduced lesions at four years. For the two teeth with enlarged radiolucency at one year, the volume of radiolucency had doubled by four years, according to the results.
Cox regression analysis showed that the size of the preoperative radiolucency influenced the radiographic outcome (p = 0.038, hazard ratio = 0.436, 95% confidence interval = 0.199 to 0.954). Teeth with large preoperative radiolucencies (volume > 65 mm³) had a 2.3 times higher risk of persistent radiolucency within four years compared to teeth with smaller lesions (volume ≤65 mm³), according to the results.
However, the study had limitations. The recall rate in this study decreased from the first to the fourth year after treatment, leading to a higher number of dropouts with unknown outcomes. Given the low rate of persistent periapical lesions after root canal treatment, larger clinical studies are needed to confirm their healing trends, they wrote.
"The volumetric changes in radiolucency on CBCT could reflect trends in the healing process and may foster early clinical decision-making," Zhang et al concluded.