DENVER - "2D is like radio; 3D is like television."
John Flucke, DDS, encapsulated the basic difference between imaging systems in a lively and well-attended presentation on Thursday in the Technology Expo at the 2016 ADA annual meeting.
 John Flucke, DDS, is a practicing dentist in Lees Summit, MO.
John Flucke, DDS, is a practicing dentist in Lees Summit, MO.His presentation, "Practical applications of cone-beam technology for the general dentist," focused on what cone-beam CT (CBCT) is and how it can be useful for a general practice. His presentation in 2015 focused more on treatments involving periodontics, endodontics, orthodontics, and other specialties, while this one was aimed at the general dentist who is curious but has not made the investment in CBCT.
Dr. Flucke was initially reluctant to invest in the technology when it first was developed and released, he noted.
"My first thought was, 'Thank goodness there are radiologists,' " he said. "3D imaging is too complicated for me."
As a general dentist, he does not focus on what he called "big, complicated cases." He did not see the value in a CBCT system.
But he quickly discovered that using CBCT was not as complicated as he initially thought.
"You don't have to be a radiologist or specialist to find uses for this technology," he said.
Seeing everything in the mouth
What convinced him to purchase a CBCT system was the need to be able to see everything in the mouth, which a 2D scanner is not able to do, Dr. Flucke noted.
At his practice, not every patient undergoes a CBCT scan, he said, but all new patients do have panoramic x-rays taken.
“2D is like radio; 3D is like television.”
"I only break out the CBCT machine when I know I need to see everything," he said.
Sometimes with 2D images, the reality of what a dentist might find once a procedure has started might be different than what was seen on the image, he said.
"If you don't have all the information, the reality can be completely different," he said. "If you could rotate the view, you might have a different situation than you thought you had."
This led to one of his points of emphasis: A CBCT system can be used to eliminate surprises in a general practitioner's practice.
"It's a whole lot easier not to have problems in the first place," Dr. Flucke told the audience. "You don't know what you don't see."
Slices
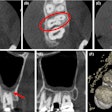
Dr. Flucke then broke down how a CBCT system and software creates the images. He said that the "tomo" in tomography means "slice."
"The device allows us to take imaging slices of our patients which can then be reassembled," he explained.
As the device rotates around the patient, it takes a series of individual images or slices. Software is used to put the images together to create the 3D volume of the image.
"Each individual image looks like a radiograph," Dr. Flucke said. "These pictures are loaded in the imaging software, which takes individual pieces of data, finds common points in them, and merges the images."
Just as with your television or computer screen, the more pixels (picture element), the better the picture looks. CBCT does not contain pixels but rather voxels. Pixels are square, while voxels are cubes, he said. The one drawback is that the more voxels, the greater the radiation dosage. However, the CBCT device puts out a "ridiculously low radiation dose," he added.
There are two types of these devices: fan beam and cone beam. Fan beam is a medical-grade imaging system that looks at all tissues, not just soft tissues like cone beam, and also puts out more radiation than a CBCT system, according to Dr. Flucke.
"If you want detail, it makes sense to have a higher number of voxels," he said. "But bread and butter implants might not require as many voxels."
He noted that most CBCT systems have adjustable detail levels, and he reminded the audience to not set their scanner on one detail level and leave it there.
The end of 2D?
For all its benefits, 3D imaging is not the be-all and end-all, Dr. Flucke said. He noted that 200 to 300 2D images are taken each day in his multipractitioner practice. Panoramic x-rays have some advantages as well.
"2D definitely has a place in dentistry," Dr. Flucke said. "There's no end date to the use of 2D right now."
But, he said, if a practitioner is doing information gathering before treatment planning, why leave out the most comprehensive data-gathering step?