Imaging aided in diagnosing a man with methicillin-resistant Staphylococcus aureus (MRSA) bacteria and a spinal infection likely caused by a dental infection. The case report was published on December 6 in the Cureus Journal of Medical Science.
After receiving antibiotics, the 54-year-old’s health improved. However, he left the hospital against medical advice. This report showcases the importance of considering dental infection as the origin of bacteria and spinal infections, the authors wrote.
“Since he presented with bacteremia and a spinal infection, it is likely the patient had an infection in the oral cavity that spread hematogenously to the blood, and then the spine,” wrote the authors, led by Dr. Nicholas Munoz of Temecula Valley Hospital in California.
A 54-year-old man with severe pain
The man -- who had a history of Crohn’s disease, gout, asthma, and arthritis and a history of smoking heroin -- presented at a hospital with severe neck and back pain. His Crohn’s disease caused periodontal and endodontic disease. Also, the man had active dental caries and told doctors he had chronic tooth pain since his 20s and had not been to a dentist in 24 years, the authors wrote.
The man underwent computed tomography (CT) imaging of the spine, which showed no signs of infection, but tests showed he had an elevated white blood cell count. The patient was discharged with muscle relaxers and told to follow up with his primary care doctor.
Several days later, tests revealed that his blood was positive for MRSA bacteria. The man was told to return to the hospital. When he returned, he reported having fevers and chills along with back pain. Furthermore, he reported previously having neck stiffness and numbness and tingling in his right foot that radiated to his thigh, they wrote.
Months prior to his hospitalization, two of his molars fell out, and since then, the man had increasing pain on the left side of the jaw that radiated to the back of the neck. The pain slowly migrated from his neck to his lower back, impairing his ability to work.
The patient told doctors he had a history of smoking heroin but had quit for over a year. Due to his pain, he started taking oxycodone, methamphetamines, and fentanyl, according to the report.
The patient was intermittently febrile with temperatures, but his heart had a regular rate and rhythm, and his lungs were clear. His lab work indicated an infection. He received five sets of blood cultures, all of which were positive for MRSA, resistant to oxacillin, and sensitive to vancomycin, the authors wrote.
A CT scan of the maxillofacial area with contrast revealed endodontic and periodontal disease involving the molars, and magnetic resonance imaging (MRI) of the lumbar spine with and without contrast showed discitis at L4-L5, with abnormal enhancement of anterior paraspinal soft tissues from L4-S2. The MRI of the cervical spine showed a soft-tissue lesion, likely an abscess, with surrounding edema and enhancement. There was no evidence of osteomyelitis, discitis, or epidural abscess in the cervical spine, they wrote.
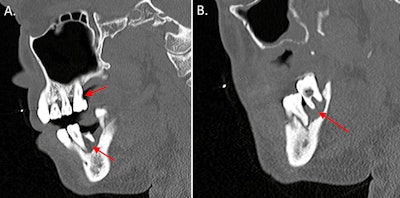 (A) A CT scan with contrast shows the sagittal view of the man's endodontic and periodontal disease of the right teeth (red arrows). (B) A CT scan with contrast shows the sagittal view of the patient's periodontal disease of the left teeth (arrow). Images courtesy of Munoz et al. Licensed by CC BY 4.0.
(A) A CT scan with contrast shows the sagittal view of the man's endodontic and periodontal disease of the right teeth (red arrows). (B) A CT scan with contrast shows the sagittal view of the patient's periodontal disease of the left teeth (arrow). Images courtesy of Munoz et al. Licensed by CC BY 4.0.
Initially, the man was started on IV vancomycin, ceftriaxone, ampicillin, and metronidazole. After the patient's workup was completed, the differential diagnosis was narrowed to arachnoiditis, periodontal infection, endodontic infection, bacteria, and paraspinal abscess.
After a consultation with the infectious disease team, the patient was only given vancomycin. The team determined there was a high probability that a dental infection led to MRSA in the patient's blood, which was the causative organism of his spinal infection.
 An MRI with contrast of the man’s cervical spine revealed a soft-tissue lesion likely reflecting an abscess with surrounding edema and enhancement (red arrows).
An MRI with contrast of the man’s cervical spine revealed a soft-tissue lesion likely reflecting an abscess with surrounding edema and enhancement (red arrows).
His fever resolved and his pain improved with treatment. A few days later, the man was found in possession of a lighter and a bag of white powder that was suspected to contain illegal drugs. The man fled when hospital security called the sheriff's department.
Head, neck infections often linked to dental problems
Most infections of the head and neck are odontogenic. They can lead to complications such as sepsis, necrosis, and endocarditis. Factors such as diabetes, alcohol use, and immunodeficiency can exacerbate the severity of dental infections. Therefore, it is critical to find the origins of infections, they wrote.
“It is possible the patient's infection spread through contiguous tissue spaces to the spine although it is more likely the infection spread hematogenously from the oral cavity to the blood, and then to the spine as the patient had MRSA bacteremia,” Munoz et al wrote.