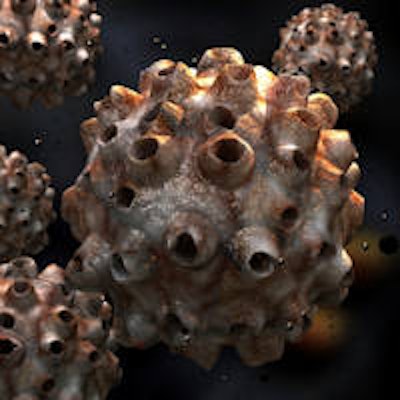
Head and neck surgeons are knowledgeable about the human papillomavirus (HPV) and show generally positive attitudes and beliefs about HPV education and vaccination, according to a new study in JAMA Otolaryngology--Head & Neck Surgery (August 29, 2013).
However,68.9% reported that their daughters had received or would receive the HPV vaccine, while 55.8% reported that their sons had received or would receive the vaccination.
The relationship of HPV to oropharyngeal cancer is now well-established, with 40% to 80% of cases of oropharyngeal squamous cell carcinoma (OSCC) in the U.S. estimated to be related to HPV, noted the U.S. team of researchers. The incidence of OSCC has been increasing over the past 30 years in many parts of the world, a trend now attributed to the HPV epidemic.
In the U.S., the incidence of HPV-positive OSCC increased by 225% between 1988 and 2004, compared with a 50% decline in the incidence of HPV-negative OSCC. Recent epidemiologic evidence indicates that the prevalence of oral HPV infection is associated with an increased number of lifetime sexual partners.
Head and neck surgeons play a critical role in detecting and treating HPV-related OSCC, and they are arguably the best poised to educate patients, families, and the public
regarding the prevention of the disease, the study authors noted.
20-question survey
For this study, the researchers surveyed 1,081 members of the American Head and Neck Society (ANHS) in late 2011 and early 2012 regarding their knowledge, attitudes, and current practices regarding HPV education and vaccination.
A total of 297 (27.5%) completed the 20-question survey. A majority of the respondents were male (86.2%), fellowship-trained head and neck surgeons (80.4%), and most practice in an academic setting (77.1%) in the U.S. (78.1%). The 59 respondents from outside the U.S. (21.9%) came from 25 different countries.
Of the 297 who responded, 22 declined to complete the demographic questions regarding their sex, age, training, time in practice, and practice setting.
Among the group, approximately 35% of their patients pay through Medicare, and 36.6% pay through private insurance.
A majority of the respondents (94.9%) said they routinely discuss the risk factors for head and neck cancer with their patients. Most (90.9%) also specifically mention HPV as a risk factor. However, only 160 respondents (49.1%) discuss the importance of current efforts to provide HPV vaccine to preadolescents.
When asked why they do not discuss the HPV vaccine with their patients, respondents gave various answers. The most common reason (38.7%) was they don't do it because their patients are adults. The next commonly cited reasons were that the safety and effectiveness of the vaccine have not yet been proved (16.7%), and they didn't consider it part of their healthcare role (13.5%).
The study found a statistically significant association between the practice setting (academic versus nonacademic) of the respondents and their attitudes about the role of pediatricians in HPV awareness (p = 0.01). Practitioners in an academic setting were more likely to agree that pediatricians should not be the sole source of information on the HPV vaccines than practitioners in nonacademic settings, 49% compared with 27%, respectively.
A majority of respondents agreed that it's necessary to discuss sexual issues with patients before recommending HPV vaccines (56.2%), and they agreed that efficacy and safety of new vaccines can only be established after they've been on the market for five to 10 years (59.6%).
Notably, 70.1% agreed that discussing the HPV vaccine is appropriate and helps patients.
An overwhelming majority (96.6%) support ANHS efforts to educate clinicians, increase public awareness, and educate patients about HPV vaccines.
Educating patients
HPV vaccines
Currently, two U.S. Food and Drug Administration-approved HPV vaccines are on the market: Gardasil and Cervarix.
Gardasil is effective against HPV types 6, 11, 16, and 18, and has shown efficacy in preventing cervical, anal, and vaginal cancers and genital warts. It is also the only HPV vaccine approved for males. Cervarix is a bivalent vaccine against HPV types 16 and 18.
The U.S. Centers for Disease Control and Prevention currently recommends routine HPV vaccination for girls and boys ages 11 to 12 years, although the series of three shots can be started as young as age 9. Catch-up immunization is recommended to age 26 years for women and age 21 for men.
The study found that head and neck surgeons are knowledgeable regarding HPV infection and its relationship with OSCC, and that most include HPV in discussion of risk factors with patients.
"Head and neck surgeons are on the front lines of diagnosing and treating HPV-related OSCC," the researchers noted. "They are the main source of information for patients regarding the etiology of their disease."
However, the researchers pointed out that fewer than half of the respondents routinely discuss the HPV vaccination with their patients.
The researchers surmise that head and neck surgeons don't advocate HPV vaccines with patients because they do not currently carry specific indications for the prevention of oral HPV infections, and the prevention of HPV-related OSCC hasn't been established.
"This study reveals tremendous opportunity for the AHNS and other organizations to better educate clinicians, patients, and the public regarding HPV-related OSCC and the importance of HPV vaccination," the study authors concluded.



















