While the failure rate for dental implants remains low, failures do occur, sometimes as a result of peri-implantitis. But to understand the cause of implant failure using an imaging modality, is cone-beam CT (CBCT) better than intraoral radiology for assessing peri-implant bone defects?
These are the most frequently used modalities to detect peri-implant bone defects, so researchers conducted a literature search on their accuracy. In the end, they offered a positive if lukewarm assessment of the modalities' performance, finding that both are clinically acceptable but neither technique offers high accuracy.
"Both CBCT and introral radiology showed a clinically acceptable performance for assessing peri-implant bone defects," the study authors wrote (Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, June 22, 2017).
The study was led by Lauren Oliveira Lima Bohner, DDS, a doctoral student in the department of prosthodontics at the University of São Paulo School of Dentistry in Brazil.
Accuracy a question
Peri-implantitis may lead to bone loss after prosthodontic rehabilitation and may result in the loss of osseointegration without treatment. One of the diagnostic criteria for peri-implantitis is the presence of suppuration and bleeding on probing associated with a radiographic bone loss greater than a third of the implant height. Clinically evaluating a patient's bone condition during the follow-up of implant placement is essential, the study authors noted.
“Both CBCT and intraoral radiographyshowed a clinically acceptable performance for assessing peri-implant bone defects.”
But when it comes to imaging these bone defects, there is no consensus in the literature about which technique is the most accurate for evaluating the bone surrounding dental implants.
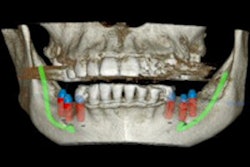
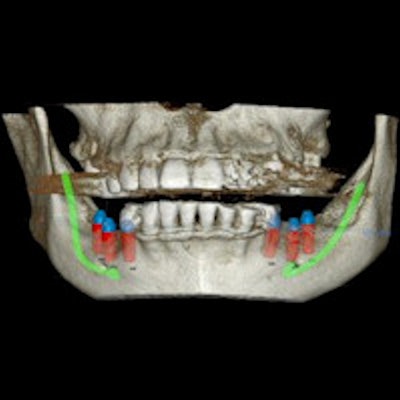
Radiography is the most common technique used to diagnose peri-implantitis, the authors noted. But both intraoral and panoramic radiography only offer 2D images of the peri-implant bone, while CBCT offers a 3D view. The limitations to these techniques include cost, radiation exposure, and presence of metal artifacts.
The researchers sought to systematically review the published literature regarding the diagnostic accuracy of imaging techniques in detecting peri-implant bone defects.
Beginning with 680 articles published from 1991 to 2016, the authors winnowed the number to 12 eligible studies. These studies evaluated the use of CBCT, intraoral radiography, computed tomography, or panoramic radiography in detecting peri-implantitis.
The authors compared sensitivity (the chance that the test will identify a condition if present) and specificity (the chance that a test will reveal if the patient is free of a condition). A rate above 80% was considered excellent, 60% to 80% was good, and below 60% was poor. For CBCT, the pooled sensitivity from the studies was 59%, while the pooled specificity was 67%. For intraoral radiography, the pooled sensitivity was 60%, and the pooled specificity was 59%. The authors noted that these values are considered clinically acceptable, the authors noted.
"When considering 60% as the threshold between poor and good outcomes, these results suggest that the techniques do not present a high accuracy, although they might be considered clinically acceptable," the authors wrote.
Advantages don't add up
The authors noted several limitations in the studies, including a high risk of bias for patient selection, meaning the studies did not offer a randomized sample or were designed as a "case control" study. The explanations for these limitations might be that some of the studies were in vitro studies, which prevents randomization, and that a case control process was necessary to see if a peri-implant defect was present.
While CBCT offers the advantage of 3D images, it was no more effective in finding these bone defects than intraoral radiography, the authors concluded.
"Despite the better visibility provided by three-dimensional images, the results of eligible studies suggested that the performance of CBCT was lower or at least comparable with that of intraoral radiography," they wrote.