
A woman was treated successfully for severe facial skeletal deformities caused by the condylar resorption of her temporomandibular joint, which stemmed from childhood trauma. The report was published on August 13 in Oral and Maxillofacial Surgery Cases.
Oral surgeons in California used multiple procedures, including a LeFort I osteotomy, a sagittal split mandibular osteotomy, and an anterior iliac crest bone graft, to correct the 38-year-old woman's dental deformities. She was treated without having her temporomandibular joint replaced or experiencing any significant complications, the authors wrote.
"Supporting the use of inverted-L osteotomy and iliac bone graft can be considered a good alternative for the treatment of mandibular deficiencies," wrote the group, led by Dr. Derek Vajda from the Division of Diagnostic and Surgical Sciences at the University of California, Los Angeles.
 A composite of the patient, showing significant facial asymmetry and malocclusion prior to surgery. All images courtesy of Vajda et al. Licensed under CC BY 4.0.
A composite of the patient, showing significant facial asymmetry and malocclusion prior to surgery. All images courtesy of Vajda et al. Licensed under CC BY 4.0.Vital and vulnerable
The mandibular condyle is necessary for proper growth of the jaw and is highly vulnerable to deformity because it is a site of compensatory growth. Specifically, the condyle responds to the functional demands of its surrounding soft tissue.
Trauma to the condyle in childhood can negatively affect opening of the mouth and facial symmetry. Unfortunately, correcting these conditions can be complex and often requires orthognathic surgery along with orthodontic and prosthodontic treatments.
In the current case, the woman at age 2 experienced trauma to the right side of her face. By age 11, she had progressively worsened dental occlusion and facial asymmetry that affected her ability to chew. At that time, the woman was diagnosed with severe maxillomandibular deformity with functional deficits, as well as pain secondary to her right jaw failing to grow, according to the authors.
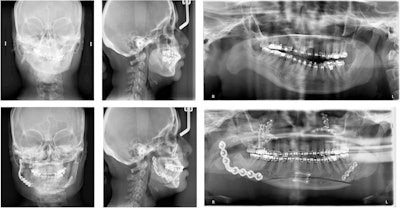 The patient's presurgery cephalometric radiograph.
The patient's presurgery cephalometric radiograph.In July 2017, the woman visited the oral and maxillofacial surgery clinic due to her poor bite and facial asymmetry. A physical exam revealed that she had a severe 10-mm occlusal cant, only contacting on her right premolars and molars, with a left-sided open bite. This caused a 2-mm incisal display in repose and a negative 2-mm gum display when she smiled. When smiling, the cant caused a 3-mm gingival display on her left and a negative 4-mm gingival display on the right. Also, her chin deviated dramatically to the right of the midline of her face, the authors wrote.
At the end of the appointment, she was referred to orthodontics for presurgery leveling, aligning, overcrowding correction, and dental decompensation. Six months prior to surgery, the woman's first premolars and remaining third molars were extracted.
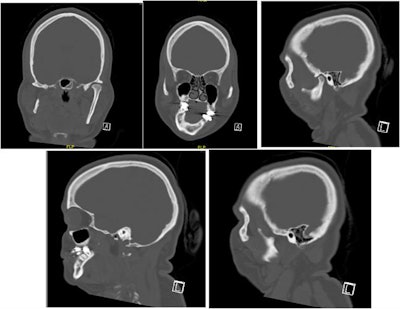 Selected computed tomography (CT) scan slices show mandibular and maxillary hypoplasia and condylar resorption on the right side.
Selected computed tomography (CT) scan slices show mandibular and maxillary hypoplasia and condylar resorption on the right side.In December 2020, she was placed under general anesthesia and underwent the following procedures:
- LeFort I maxillary osteotomy
- Right mandibular inverted L ramus osteotomy
- Left mandibular sagittal split ramus osteotomy
- Genioplasty
- Reconstruction of the right mandibular ramus
- Right zygomaticomaxillary buttress with an anterior iliac crest bone graft
Her procedures went well. For four weeks, maxillomandibular fixation was maintained. Guiding elastics were then used until the seventh week. At that time, the woman's face was largely symmetrical, and she was healing without complications.
After the procedures, the woman was seen every week for eight weeks and then at three months. At the three-month appointment, clinicians found that she had developed a 2-mm anterior open bite with equal contacts on her second molars. Using orthodontic intrusion, the open bite was closed, the authors wrote.
 Images of patient three months after surgery.
Images of patient three months after surgery.Reasoning behind the strategy
The severity of the woman's skeletal malocclusion greatly increased the complexity of her reconstruction, and several treatment options were considered, the group noted. Many surgeons likely would have chosen to reconstruct her right temporomandibular joint with an alloplastic joint replacement or costochondral graft reconstruction.
In this case, they chose to perform an inverted L osteotomy without joint reconstruction because the patient's existing fibro-articulation had a good pain-free range of motion, and she had no temporomandibular joint-associated symptoms.
"Even in the setting of a missing condyle, condylar reconstruction is not always necessary, especially without condylar symptoms and with good condylar function," Vajda and colleagues wrote.




















