
Clinicians used lingual compression to assist a 40-year-old woman who experienced a severely enlarged tongue, almost stretching to her chest, following prone positioning as part of COVID-19 treatment, according to a case report published on July 16 in BMJ Case Reports.
The doctors chose the novel treatment of wrapping the woman's tongue with gauze and a compression wrap for multiple days after other interventions failed. Lingual compression may be safely used when macroglossia is unmanageable or removing part of the tongue is being considered, the authors wrote.
 View of the lingual compression wrap. All images courtesy of Adam M. Ackerman, MD, et al.
View of the lingual compression wrap. All images courtesy of Adam M. Ackerman, MD, et al."Application of a lingual compression was effective in resolving macroglossia while avoiding the need for partial glossectomy," wrote the group, led by Adam M. Ackerman, MD, of the department of surgery at Henry Ford Hospital in Detroit.
Acute macroglossia is a rare clinical problem that has been linked to trauma, medication side effects, allergic reactions, patient positioning, pressure packing of the oropharynx, and oral surgery. Extreme cases may compromise a person's airway and lead to speech and swallowing difficulties. It is often managed with steroids and bite blocks, but when that doesn't work, clinicians must consider a partial glossectomy. However, removing part of the tongue has been associated with postoperative speech and swallowing problems.
40-year-old woman
In this case, the patient presented at the hospital emergency room after experiencing a week of fever, shortness of breath, and diarrhea. She tested positive for COVID-19 and had a medical history of insulin-dependent diabetes, pancreatic insufficiency, asthma, high blood pressure, and ulcerative colitis.
The woman was intubated after her respiratory function worsened quickly despite breathing treatments. She was given a combination of hydroxychloroquine, methylprednisolone, and tocilizumab. She developed serious, persistent hypoxia and acute respiratory distress syndrome despite treatment.
The patient's ratio of partial pressure of oxygen to fraction of inspired oxygen was less than 100, so attempts were made to improve her oxygenation using prone positioning treatment. The hospital's protocol is 16 hours of prone positioning, followed by eight hours of supine positioning. Though the positioning caused worsening lower facial swelling and macroglossia, improving the patient's oxygenation was deemed more important.
Preserving the tongue
At the end of the 11-day positioning treatment, the woman's tongue was nearly capable of resting on her chest, according to the authors. Her macroglossia was attributed to the prolonged positioning treatment.
After consultation with the otolaryngology department, the woman was given an additional 10-day course of methylprednisolone in addition to a bite block. This had a minor impact; the patient's tongue remained significantly swollen with an excessive amount of fluid and protruded from her mouth. The patient also developed pressure injuries over the ventral surface, where the tongue was in contact with teeth and the endotracheal tube.
Doctors performed a tracheostomy on the woman during day 26 of her hospital stay, and the next day, lingual compression was applied to avoid having to remove part of her tongue. The woman's tongue was wrapped loosely with saline-moistened gauze, and an elastic, self-adherent wrap was placed on top. At first, it was applied once daily and left on for 12 hours. Noticeable improvement was observed after the first wrapping. She continued to improve, but swelling would worsen during the 12 hours when the tongue wasn't wrapped.
On day 8 of treatment, lingual compression was applied twice daily for eight hours, followed by four hours without lingual compression. On day 11, lingual compression was discontinued because the woman could put her tongue into her mouth without difficulty.
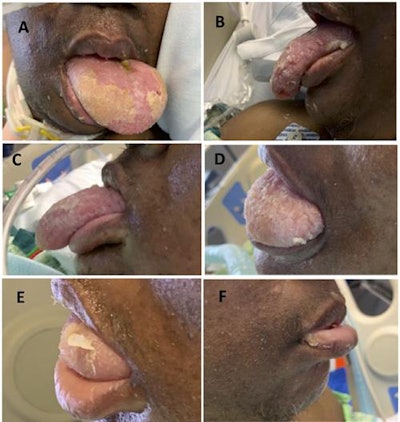 How the patient's macroglossia resolved over time with lingual compression. (A) The first day of treatment prior to wrapping the tongue. (B) The third day of treatment. (C) The fourth day of treatment. (D) The 10th day of treatment. (E) The 13th day of treatment. (F) The 14th day of treatment.
How the patient's macroglossia resolved over time with lingual compression. (A) The first day of treatment prior to wrapping the tongue. (B) The third day of treatment. (C) The fourth day of treatment. (D) The 10th day of treatment. (E) The 13th day of treatment. (F) The 14th day of treatment.The woman was discharged to a long-term assisted care facility on day 52 of her hospital stay. The macroglossia left no lasting injuries to her tongue, the authors wrote.
"[Nonoperative] management strategies may be a desirable alternative given the potential for postoperative morbidity," they wrote.




















