Soon you might be treating your patient's caries with a collagen sponge filled with a drug -- first tested to treat Alzheimer's patients -- that stimulates the natural ability of teeth to restore dentine.
A study published January 9 in Scientific Reports by researchers in the U.K. documented a new method of stimulating the renewal of living stem cells in tooth pulp. While still needing human clinical trials, this approach may allow large cavities to be repaired without the use of cement or fillings.
"The simplicity of our approach makes it ideal as a clinical dental product for the natural treatment of large cavities, by providing both pulp protection and restoring dentine," stated lead study author Paul Sharpe, PhD, in a press release. "In addition, using a drug that has already been tested in clinical trials for Alzheimer's disease provides a real opportunity to get this dental treatment quickly into clinics."
Sharpe is the head of the craniofacial development and stem cell biology division at the King's College London Dental Institute.
3 antagonists
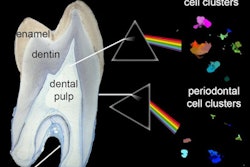
After removing caries decay, a tooth's soft inner pulp is exposed, and a natural dentine repair process begins. This process uses a form of stem cells in the patient's mouth that becomes new cells. These cells release a form of reparative dentine, according to the study authors.
“The simplicity of our approach makes it ideal as a clinical dental product for the natural treatment of large cavities, by providing both pulp protection and restoring dentine.”
Unfortunately, this process does not work to repair larger caries, hence cements and filling are used. The researchers wanted to see if a new approach that stimulates the natural formation of reparative dentine by mobilizing stem cells in the tooth pulp could work in larger caries.
They used a biodegradable collagen sponge (Kolspon, Medira) to first deliver low doses of three small-molecule glycogen synthase kinase (GSK-3) antagonists directly to maxillary molars in laboratory mice with 0.13-mm holes drilled in them to expose the pulp. The researchers theorized that dentine will replace the sponge over time and rapid, natural tooth repair will take place.
The first part of the study was to confirm success of the delivery method. The following antagonists were used:
- BIO ((2′Z,3′E)-6-Bromoindirubin-3′-oxime)
- CHIR99021 (6-[[2-[[4-(2,4-Dichlorophenyl)-5-(5-methyl-1H-imidazol-2-yl)-2 pyrimidinyl]amino]ethyl]amino]-3-pyridinecarbonitrile)
- Tideglusib (4-Benzyl-2-(naphthalen-1-yl)-[1,2,4]thiadiazolidine-3,5-dione)
Tideglusib is a pharmaceutical that is in clinical trials for systemic use in treating neurological disorders such as Alzheimer's disease, according to the study authors.
After 24 hours, the treated teeth were extracted and measured for delivery of the antagonist. The researchers determined that this was an effective delivery method, so they moved on to the second phase, in which a different set of maxillary molars had the same size holes drilled, and soaked sponges were applied for four to six weeks.
The researchers used micro-CT scanning to view and quantify mineral deposition at the drill site. At both four and six weeks, the teeth showed statistically significant mineralization with all three agonists when compared with sponge-alone controls. They reported that mineralization was, on average, twice as great as in the control group.
The researchers then sectioned each molar and used a stain to show new dentine formation. These results confirmed the imaging data that showed that more reparative dentine was formed when teeth were treated with GSK-3 inhibitors at the site.
Safe in humans
The authors noted that mouse blood volume is about 3,000 times smaller than human blood volume. However, they reported the anticipated concentrations of Tideglusib needed "would be well below that already tested in clinical trials."
"More significantly the localization of the reparative dentine formed indicated that with the treatments, the mineral replaced the biodegradable sponge and restored the cavity in the dentine made by the burr," the authors concluded.