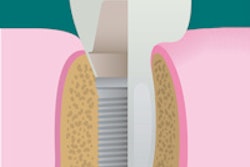
Placing implants immediately after an extraction has gained favor in dentistry, but questions remain about expectations for success. How does the timing of the procedure affect stability? And is inevitable bone loss after an extraction going to affect the implant's life span?
A systematic review examining the success rates of implants placed in fresh extraction sockets found high survival rates, according to a new study in Clinical Oral Implants Research (February 2012, Vol. 23:s5, pp. 39-66).
The examination of 46 prospective studies with an average follow-up time of 2.08 years revealed that immediate implants had an annual failure rate of 0.82% and a two-year survival rate of 98.4%. Five factors were considered to determine their influence on survival rates, and the regimen of antibiotics used after the surgery was the only one that proved significant in the study conducted by researchers from the University of Hong Kong's Faculty of Dentistry.
The aesthetic results were less reliable: 20% had less than optimal outcomes stemming from buccal soft-tissue recession.
Previous trials considered by the authors offered insufficient evidence as to which type of implant -- immediate, early, or late -- had the most significant advantages. "Therefore, the main objectives of this systematic review are to quantitatively estimate the survival and success rates of immediate implants and the implant-supported prosthesis, the prevalence of biological, technical, and aesthetic complications, and the magnitude of soft- and hard-tissue changes following implant placement in fresh extraction sockets," they wrote.
Importance of antibiotics
To obtain their data, researchers scoured Medline and the Cochrane Library using relevant search terms for the time frame of January 1991 to July 2010. Of 5,887 titles found in their initial search, 46 were selected (all but three were published after the year 2000).
“Secondary to the prescription of an effective antibiotic, the duration of usage might be of importance.”
In total, 2,130 patients between the ages of 18 and 94 with 2,908 immediate implants were considered for the study; 58 implants failed. Additionally, antibiotics were prescribed in 33 of the 46 studies.
Those studies that offered a longer follow-up time were analyzed separately, and researchers noted a four-year implant survival rate of 97.5%. "This percentage is comparable to the 96.8% five-year survival rate of implants supporting single crowns reported in a previous systematic review," the researchers wrote.
Five variables were examined in the course of the study. In particular, the use of antibiotics influenced the success of immediate implants. When comparing subjects who had received a single dose preoperatively, five to seven days postoperatively, and a single dose preoperatively plus a course of antibiotics five to seven days postoperatively, the estimated failure rates were 1.87%, 0.51%, and 0.75%, respectively, the researchers found.
One dose was not enough to effectively fend off infection during the healing period, but antibiotics administered for five to seven days after surgery may have improved the likelihood of success. "This demonstrated that secondary to the prescription of an effective antibiotic, the duration of usage might be of importance," they noted.
Sites with a history of periodontal disease were evaluated for their likelihood of failure. While it had an impact, researchers only observed a slightly higher rate of failure in those circumstances. Comparatively, the the implant site had even less of an impact. The failure rates between implants located in the maxilla and mandible were 0.73% and 0.5%, respectively; these figures were statistically insignificant.
"One possible explanation could be that most of the studies adhered to a strict surgical protocol, where immediate implants were installed with a minimal insertion torque, and 3-4 mm apical bony engagement was ensured," the researchers wrote.
They also suggested that surgical protocol was responsible for the negligible difference in failure rates between anterior versus posterior implant sites.
Loading, they determined, was insignificant as well.
Aesthetic risks
Aesthetic complications were an acknowledged drawback of the immediate implant technique. "Soft-tissue alterations, especially in the buccal marginal mucosal recession, appeared to be inevitable," they wrote.
In two studies with follow-up times of three years or more, 20% of the patients had less than ideal implant aesthetics as a result of buccal soft-tissue recession. In another, gingival recession led to 11% of patients responding that they were unsatisfied with the appearance of their implants.
"The current evidence indicated that implants placed in extraction sockets were not able to prevent soft-tissue loss, especially the buccal marginal tissue recession," the study authors wrote.
As a result, they urge cautious planning and careful case selection when preparing for immediate implant indications. Some evidence suggests that immediate restoration after immediate implant treatment could help reduce buccal mucosal recession, they noted, but more data are needed.