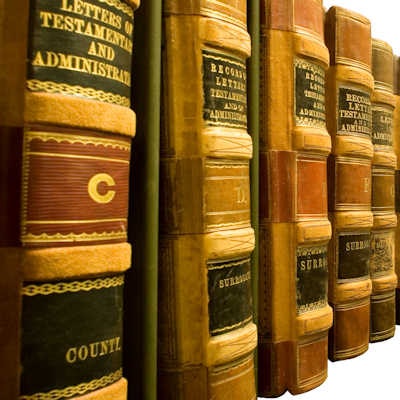
DrBicuspid.com is pleased to present the next column from two lawyers who spend every day defending dentists in litigation and before the licensing board. The purpose of this column is to offer our readers a fresh perspective on common practice and risk management issues from attorneys who litigate these issues in the real world.
A 61-year-old male patient presented to a large group practice where our client, a prosthodontist, worked one to two days per week. Our client had formal training in dental implant restoration in his residency training program, and he later took continuing education coursework in implant placement; his practice includes both the placement and restoration of implants.

On the patient's initial presentation to the office, he was seen by a general dentist, who did an overall evaluation and treatment plan. The patient was edentulous on the upper left, distal to tooth #11, and he needed only minor treatment of some carious teeth elsewhere in the mouth.
A panoramic x-ray, which was of less-than-ideal quality, was taken that day, as well as several periapical and bitewing films that are not relevant to the issues here. The examining dentist believed that the patient could benefit from having up to four implants in the upper left quadrant, as the remainder of the mouth was fully dentulous or adequately restored with bridgework.
The general dentist set up an appointment for the patient to see our client for implant placement, without ever discussing the case with our client. The plan was also for our client to do the restorations after the implants osseointegrated.
The patient presented to our client the following week, expecting to have implants placed. Our client examined the patient and reviewed the panoramic radiograh. The radiograph did not provide a very clear view of the upper left quadrant, but it was adequate enough to allow our client to measure the height of bone -- which he did with a periodontal probe -- and to determine that four implants could seemingly be placed into the area, which had varying heights of bone that measured, at least two-dimensionally, in the 8- to 10-mm range. Our client, feeling pressured by both the patient and his boss, opted against sending the patient to an outside facility for a cone-beam CT scan and instead used only the panoramic radiograph and his clinical assessments for measurement purposes.
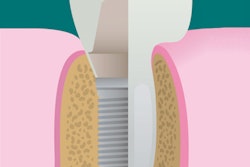
That day, our client presented the patient with an implant consent form, which contained those risks typical of the procedure. The patient read the form, had his few clarification questions answered by our client, and signed it. Our client made note of the "consent" interactions with the patient and included the signed form in the chart. With local anesthesia, our client placed four implants, all 10 mm in length, into the left maxilla. He knew that two of the implants would likely project beyond the bony floor of the maxillary sinus, but he intended that to be the case, hoping to obtain bicortical stabilization. Unfortunately, he did not record that in the chart.
The postoperative period was uneventful for the first two months, but the patient then developed an upper respiratory infection, which led to left maxillary sinusitis. He sought care from an ear, nose, and throat (ENT) physician, who treated the patient with antibiotics. The ENT also told the patient -- based on radiographs taken -- that two of his implants were projecting into the sinus. The ENT never related the sinusitis, either verbally to the patient or in his chart entries, to anything other than the respiratory tract infection. The sinusitis was persistent, despite antibiotic care, and the patient claimed ongoing breathing difficulty, headaches, and discomfort, which never went away. He never returned to our client after the one-week suture removal visit, but he instead had all four implants, which integrated well, restored by another dentist.
Legal stance
The patient filed an action against our client, claiming that he had departed from the standard of care in the following ways:
- In failing to obtain proper radiographs before placement of implants
- In failing to obtain adequate informed consent
- In improperly placing two of the implants superior to the bony sinus floor, so as to cause persistent sinusitis and related symptoms
Included in the claim were the costs of the ENT's treatment and the increased dental costs in restoring the implants, because the dentist who did the restorations charged a higher fee than our client would have. Of course, pain and suffering for "permanent lasting effects of the sinusitis" was claimed as well.
Issues raised
- X-rays: An ongoing issue that we see in implant litigation is what constitutes adequate radiographs before implants are placed. Invariably, plaintiffs and their attorneys argue that the dentist is unable to get a true sense of the bone that is available to accommodate implants without 3D imaging.
While there are certain circumstances -- the most significant of which is assessing the bone available superior to the inferior alveolar nerve in posterior mandible cases -- in which the precision provided by 3D imaging is necessary, many other circumstances do not require it, and our experts tell that to us repeatedly, backed up by literature. However, that does not stop plaintiffs from making the claim, which is often red meat for juries.
In this situation, our client was accurate in his assessment of bone height, and he planned to penetrate beyond the bony floor, so the necessity for 3D imaging was not a clinical consideration of importance. - Informed consent: From our perspective in defending the case, our client could not have done a much better job in this respect. He had an interactive discussion with the patient that was documented in the chart by our client, and the patient signed a form that documented that he had been aware of what he was getting into before he agreed to do so.
- Ideal implant placement: Our experts consistently advise us that implants in situations like this will work as well if they go beyond the bony floor of the sinus by up to as much as 3 mm to 4 mm as if they are fully encased in maxilla and with no side effects. In fact, some of our experts teach their students that it is preferable to engage the bony floor of the sinus -- for bicortical stabilization -- and extend slightly beyond it, as compared with placing a short implant fully in bone. There is no doubt that it is a potent picture for a jury to see an implant projecting into what appears to them to be "thin air," but that does not make it improper. It is our job to educate the jurors to think beyond their lay common sense.
Result
With strong expert support and a client who sincerely believed that he had acted properly across the board, we took the case to trial. As expected, the plaintiff's attorney had enlargements of x-rays that showed the tips of two of the implants projecting into the sinus cavity, mostly for the emotional effect on the jury. His expert also claimed that placing an implant "into the sinus" is malpractice.
However, on cross-examination of plaintiff's expert, he defined "into the sinus" to mean not only through the bony floor but also piercing the Schneiderian membrane, and he was unable to point to any evidence to show that the implants had, in fact, pierced the membrane. Furthermore, he was forced to admit, with regard to causation of the claimed injuries, that the ENT records did not place the cause of the sinusitis as the implants, but rather as the upper respiratory infection.
Regarding the issue of informed consent, the plaintiff admitted that he had signed the form but could not recall any discussion with our client. His expert agreed that having a patient sign a form that explained what this form did, together with a discussion between doctor and patient, met the standard of care, so the judge dismissed that claim at the close of the plaintiff's case.
Our expert explained the concept and benefits of achieving bicortical stabilization, especially in less dense bone, and explained that he often strives to place implants beyond the bony sinus floor just for this purpose, as the defendant did here. He concurred with the plaintiff's expert that there was no evidence of the membrane having been pierced, but he went past that to explain that, even if it did pierce the membrane, that would not be a problem, as evidenced by screws (made of essentially the same material as implants) being routinely placed through the membrane and into the sinus cavity for repair of midface fractures and orthognathic surgery.
Next, he focused on the fact that the subsequent treating dentist was able to use all of the implants as had been originally planned, showing that they had fully integrated and were causing no sinus problems, because dentists would not make implants part of their restorative treatment design if they were the cause of persistent sinusitis. And finally, he explained that, while the ENT noted that two implants did project beyond the sinus floor, the ENT related the sinusitis to an unrelated infection.
The jury returned a verdict in favor of our client in a relatively short time.
Practice tips
- Patient follow-up: In this case, the plaintiff was never heard from after his sutures were removed, until he filed suit. Perhaps legal action could have been avoided if the patient had been contacted and asked to return to see how he was doing. When dentists treat patients in their own practices, they can and should institute follow-up as is appropriate to the circumstances. But when dentists work for other offices -- especially as itinerants -- they can lose control over follow-up if the office does not have a system in place, so it is incumbent on such dentists to keep in touch with patients to follow and assess their progress. It stands to reason that patients who believe that their dentist cares about them are less likely to sue even when the results are not as desired.
- Documentation: As we have discussed in prior articles, it cannot be emphasized enough just how important chart entries are. Here, if our client had documented in the chart, on the day of implant placement, that he intended to place two of the implants beyond the bony floor of the sinus, we would not have had to explain that away at trial.
Our client thought about doing this before he did it, he planned to do it, and he did what he planned, so putting that all in writing legitimizes that a thought process was behind his actions, as compared with possibly appearing that an excuse was being made after the fact. We are not suggesting that chart notes need to be lengthy and time-consuming narratives, but they do need to include the procedure details, the informed consent process, rationales for treatment or nontreatment, and anything that might otherwise raise an eyebrow. Write every chart entry as though a jury might someday be reading it. - Realize who has ultimate patient responsibility: Regardless of where a patient is treated, the instrumentation available to a treating dentist, and time and financial pressures that may be placed upon a dentist by outside sources under a given set of circumstances, the standard of care is not altered, and it must be met so as to comport that which is dentally reasonable and appropriate. The last thing a dentist should ever have to say is that he or she compromised patient care to satisfy an employer. The treating dentist is responsible primarily, with the employer's responsibility being secondary, and then only sometimes.
William S. Spiegel, Esq., is a partner at the law firm Spiegel Leffler in New York City. He is a former assistant corporation counsel to the City of New York -- Medical Malpractice Division.
Marc R. Leffler, DDS, Esq., is also a partner at Spiegel Leffler. He received his dental degree from Columbia University, completed a residency in oral and maxillofacial surgery at New York University, and is a diplomate of the American Board of Oral and Maxillofacial Surgery.
Disclaimer: Nothing contained in this column is intended as legal advice. Our practice is focused in the state of New York, and there are variations in rules of practice, evidence, and procedure among the states. This column scratches the surface on many legal issues that could call for a chapter unto themselves. Some of the facts and other case information have been changed to protect the privacy of actual parties.
The comments and observations expressed herein do not necessarily reflect the opinions of DrBicuspid.com, nor should they be construed as an endorsement or admonishment of any particular idea, vendor, or organization.