A humanized antibody used in cancer immunotherapy may be associated with a 44-year-old woman developing osteonecrosis of the jaw (ONJ). The case report was published on January 1 in Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.
Jaw osteonecrosis, which generally is not associated with immunotherapy, may be a "rare yet possibly emerging complication" of pembrolizumab therapy. This is only the second reported case of ONJ associated with pembrolizumab, which is being used in the treatment of more than 20 cancers, the authors wrote.
"In patients that exhibit oral and systemic symptoms related to their immunotherapy, care should be taken to reduce potential trauma to the oral cavity," wrote the authors, led by Dr. SaeHee Yom, MPH, of Memorial Sloan Kettering Cancer Center in New York City.
A 44-year-old woman with a painful gum lesion
In September 2021, the woman, who previously had Hodgkin lymphoma, had a cancer relapse. She had diffuse osseous hypermetabolic metastatic foci throughout her skull base as well as her axial and appendicular skeleton.
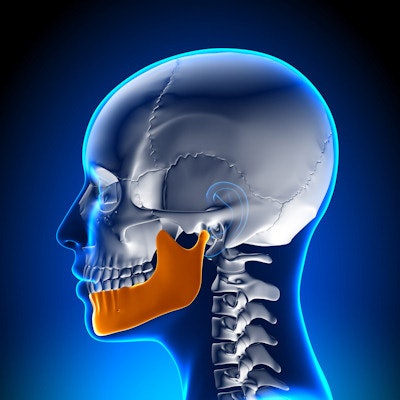
In November 2021, she started weekly treatment with gemcitabine, vinorelbine, doxorubicin, and pembrolizumab, with plans for an autologous transplant. A month later, after having undergone four doses of pembrolizumab, she went for an evaluation due to a painful gum lesion. At that time, a positron emission tomography (PET) scan revealed abnormal uptake at the lingual plate of the right jaw with cortical irregularity. In the right submandibular gland, asymmetric activity that was possibly obstructive also could be seen, the authors wrote.
The woman reported feeling pain in the mandibular right lingual gingiva and mobility of the maxillary right third molar #1 and the mandibular right first molar #30. An oral exam showed firm swelling, which extended from the floor of her mouth to the lingual occlusal table. The area was especially tender to the touch. There were no signs of discharging pus or tooth decay, according to the report.
An x-ray revealed that the bone near tooth #30 had a "moth-eaten radiolucent pattern" and slight extrusion of the tooth. Clinicians suspected the lesion was due to therapy or systemic disease. Therefore, an oral hygiene regimen and chlorhexidine rinse were recommended.
When the patient returned in January 2022, the swollen area had a 12 × 5 mm area of exposed bone. Also, the surrounding gum was inflamed. The woman had heavy plaque deposits because she stopped brushing her teeth due to the pain. She also had gingival overgrowth around several teeth, they wrote.
The area was cleaned, and she was told to return a week later for debridement as long as her blood counts allowed for it. Three weeks later, she returned, and the exposed bone area had grown to 17 x 10 mm. The entire necrotic bone segment was removed, according to the report.
She was told to maintain her oral hygiene regimen and returned four days later to undergo an autologous stem cell transplant. She had no other symptoms, and the woman was symptom-free in June 2022, the authors wrote.
Why it matters
Currently, pembrolizumab, an immune checkpoint inhibitor, is used in the treatment of lung, head and neck, stomach, cervical, colon, rectal, and some types of breast cancer, as well as melanoma and Hodgkin lymphoma. It is administered by slow injection.
In general, patients better tolerate immune checkpoint inhibitors and experience fewer oral toxicities compared to conventional chemotherapy. However, oral-related adverse events, including mucosal changes, such as gingival sloughing, and dry mouth, have been reported. Though ONJ is reported less frequently with immune checkpoint inhibitors, it has been reported with ipilimumab, they wrote.
Since the number of patients receiving this humanized antibody is likely to increase in the future, "any further instances of ONJ should be documented in order to better inform dental management around cancer patients undergoing pembrolizumab therapy," Yom and colleagues wrote.




















