The importance of the oral systemic link got another nod when a recent Columbia University study found that people with periodontal disease are more likely to have increased levels of inflammation, which is also a risk factor for cardiovascular disease (CVD).
Periodontal disease and CVD are both caused by inflammation, explained John Grbic, D.M.D., M.M.Sc., a professor at the Columbia University College of Dental Medicine and one of the study authors, in a DrBicuspid.com interview.
"The bacteria that cause periodontal disease elicit an inflammatory response in their periodontium. The cytokines produced by inflammatory cells in the periodontium can enter the circulation and cause increased inflammation in other parts of the body," he said. "These bacteria can also enter the circulation and deposit themselves in areas of atheroma formation such as coronary arteries. Periodontal pathogens have been found in arterial plaques. The presence of these bacteria can cause inflammation, leading to the formation of more atheromas."
Although this hypothesis suggests that the treatment of periodontal disease should reduce the risk of CVD, it has never been proved in an interventional trial. However, studies have shown that treatment of periodontal disease may lower levels of circulating inflammatory mediators, Dr. Grbic said.
Also, patients with increased generalized systemic inflammation may be vulnerable to diseases caused by inflammation, including CVD and periodontal disease, he added.
"Of course, the relationship may be a combination of both of these possible mechanisms," Dr. Grbic said.
The Columbia University Medical Center study involved 421 individuals who did not have heart disease but were family members or cohabitants of patients with heart disease. They were screened for traditional CVD risk factors and also answered questions about their oral health (American Journal of Cardiology, December 1, 2008, Vol. 102:11, pp. 1509-1513).
Researchers noted that, in a diverse population of individuals eligible for the primary prevention of CVD, a history of periodontal disease was associated with significantly higher levels of Lp-PLA2, an inflammatory marker, when compared to those without periodontal disease. The data indicates a possible association between oral health and inflammation, which in turn means that inflammation could be a factor in the relation between oral health and CVD, the authors noted.
"It is not possible to conclude from these data that oral health is a risk marker for CVD or CVD outcomes or that any therapy based on oral health status will be effective," the authors concluded. "Our data suggest that 'at-risk' individuals who may otherwise not be identified by traditional CVD risk screening might be identified through oral health screening."
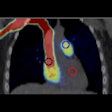
Another recent study corroborated the link between inflamed gums and periodontal disease. Researchers from the University of Milan looked at 35 healthy people who had mild to moderate periodontal disease. They examined the subject's carotid arteries at baseline and at several points over the course of periodontal treatment. One year after treatment, they observed a reduction in oral bacteria, immune inflammation, and the thickening of the blood vessels associated with atherosclerosis, the chronic inflammatory response in artery walls (Journal of the Federation of American Societies for Experimental Biology, December 12, 2008).
"It has been long suspected that atherosclerosis is an inflammatory process and that periodontal disease plays a role in atherosclerosis," said Mario Clerici, M.D., a senior researcher on the study, in a press release. "Our study suggests that this is the case and indicates that something as simple as taking good care of your teeth and gums can greatly reduce your risk of developing serious diseases."
More aggressive perio treatment?
For dentists, this discovery means they can play a key role in screening patients for potential cardiovascular problems and referring those at risk for a more through evaluation with their physician, said Dr. Grbic while discussing the results of the Columbia University study. Also, these findings indicate that physicians can determine which patients need to be screened for CVD by asking relatively simple questions about their oral health.
Does it also mean the treatment of periodontal disease should change?
"No, although it makes diagnosis of periodontal disease more important," Dr. Grbic said.
Michael McGuire, D.D.S., who addresses the inflammation link in another recent article (Journal of Periodontology, November 2008, Vol. 79:11, pp. 2016-2020), feels the link between periodontal disease and inflammation does warrant some changes in treatment, however.
Dr. McGuire warned that gingival inflammation cannot be viewed as a simple problem, especially in high-risk patients -- such as heavy smokers, diabetics, and interleukin-1 genotypes -- and those with systemic inflammatory conditions who do not respond to debridement.
These patients should be treated more aggressively, he advised. He recommends shortening their recall intervals, reinforcing home-care techniques, recommending toothpastes or essential oils with anti-inflammatory properties, and prescribing local delivery drugs, systemic antibiotics, or subantimicrobial dose doxycycline as part of the recall regimen.
"Because inflammation is associated with systemic events, why take a chance?" he wrote.
Solid links seem to exist between periodontal diseases and systemic inflammatory diseases, but it may take many years before the systemic therapeutic benefits of periodontal treatment are established, he noted.
If these benefits are established, there may be changes in the way dentists practice, such as an increase in referrals of periodontal patients with systemic conditions, inclusion of periodontal evaluation in medical protocols, and more collaboration with medicine in both patient care and research, Dr. McGuire concluded.