A 54-year-old woman lost vision in one eye after developing orbital cellulitis following a tooth extraction, according to a recent case report published in Advances in Oral and Maxillofacial Surgery.
Computed tomography (CT) scans revealed swelling and fluid around the woman's eye and partial opacification of her maxillary sinus and aided in the diagnosis of the rare but deadly bacterial infection, odontogenic orbital cellulitis. Surgery treated her infection but the woman has complete vision loss in her left eye, they wrote.
This is "a rare case of complete loss of vision secondary to odontogenic orbital cellulitis," wrote the authors, led by Dr. Aria Amir Ghasemi, of the department of otolaryngology at the University Hospital Southampton National Health Service Foundation Trust in the U.K. (Adv Oral Maxillofac Surg, October 14, 2021).
Odontogenic orbital cellulitis is a life-threatening bacterial infection that causes inflammation of the eye that is secondary to a tooth-related infection. Sinusitis and trauma are the most common risk factors for orbital cellulitis, but it also is an unusual complication of a dental infection. Often, it is caused by common types of bacteria, including Staphylococcus and Streptococcus species. In addition to blindness, untreated orbital cellulitis can spread to a person's lymph nodes and bloodstream and quickly lead to death.
After three days of left-sided periorbital swelling, nasal discharge, and increasing facial pain, the woman went to the hospital. Her symptoms began after having a tooth extracted, the authors wrote.
When she arrived, she had a rapid heartbeat and showed signs of a fever. Her left eye was protruding with extensive conjunctival hyperemia and restricted eye movements. The patient said that her vision in her left eye was increasingly blurry. After a few hours, she lost complete vision in that eye, they wrote.
To relieve pressure in her eye, lateral canthotomy was performed. The assessment revealed that there was no perception of light in her left eye. Also, in that eye, central retinal artery occlusion, which is the blockage of blood to the eye's retina, was noted. To control intraocular pressure, she was started on an ointment, intravenous antibiotics, and topical steroid drops, according to the report.
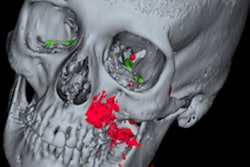
CT scans showed that her sinuses had significant preseptal and postseptal swelling with retro-orbital fat stranding with small volume fluid noted at lateral and superior left orbit, with no drainable collection in the orbit. The imaging also showed partial opacification of the patient's left maxillary sinus and anterior ethmoid air cells. The scans showed that her condition met the criteria for orbital cellulitis, they wrote.
 An axial CT scan shows significant preseptal swelling and post septal/retro-orbital fat stranding with small volume fluid at the lateral and superior left orbit. There was considerable protrusion of the left eye, as well as anterior ethmoid cell opacification. Images courtesy of Ghasemi, et al. Licensed under CC BY 4.0.
An axial CT scan shows significant preseptal swelling and post septal/retro-orbital fat stranding with small volume fluid at the lateral and superior left orbit. There was considerable protrusion of the left eye, as well as anterior ethmoid cell opacification. Images courtesy of Ghasemi, et al. Licensed under CC BY 4.0. An axial CT scan shows opacification of the woman's left maxillary sinus with marked soft tissue swelling of her left infraorbital.
An axial CT scan shows opacification of the woman's left maxillary sinus with marked soft tissue swelling of her left infraorbital.During endoscopic sinus surgery procedures, pus immediately released from her very congested maxillary sinus. Lab results showed that Staphylococcus aureus, a bacterial that can colonize in the oral cavity, caused the cellulitis, they wrote.
Though the patient's eye muscle weakness and bulging resolved three days after surgery, her vision in her left eye did not return, the authors added.
"Loss of vision in patients presenting with odontogenic cellulitis is infrequent," Ghasemi and colleagues wrote.