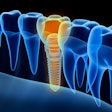
In many studies, dental implant survival rates sit comfortably in the mid 90% rate. However, it is also not unusual for studies to exclude all but the most ideal candidates for implant treatment. In a typical practice setting, clinicians dealing with a range of situations should be prepared for the possibility of the need for reimplantation.
The authors of a new study published in Journal of the American Dental Association bluntly state that, as implant therapy becomes more common, so will the need to treat those that are painful or failing (JADA, August 2014, Vol. 145:8, pp. 835-842). The number of implants placed in the U.S. is estimated to double from 1 million to 2 million implants inserted in 2010 to 2 million to 4 million by 2020, according to a 2012 Straumann report.
Data on the best strategies for how to address these situations are both available and still arriving. Consequently, researchers from the Columbia University College of Dental Medicine in New York City decided to review the available literature published within the last two years in regard to failing dental implants. Their observations can help clinicians create a plan of action for responding to failing implants and set expectations for themselves and their patients.
"The decision to remove an implant needs to be based on clinical assessments, radiographic evaluations, or both," wrote study authors Gary Greenstein, DDS, and John Cavallaro, DDS. "Reimplantations can be performed successfully, but their survival rate appears to be lower than half of implants placed at sites from which they were not lost formerly."
They noted rates of survival reported in the literature after the second and third implantation in the same site ranged from 71% to 100% and 50% to 100%, respectively.
"There were scant data addressing implant survival after second reimplantations" or a third implant placed in the same site, the authors noted. Furthermore, the studies with 100% success rates involved very small groups of implants.
While a surviving implant may not be a "successful" one, what exactly constitutes a "failing" implant is arguably the most important implant definition, since it necessitates removal. Implants in this group have "pain on function, mobility, radiographic bone loss of more than one-half the length of the implant body, and uncontrolled exudate," the authors explained.
The researchers also issued a warning about the occurrence of "cluster failures," when a single patient has multiple failing implants. According to the data, these types of failures happen not long after implantation and are an indication of problem specific to that particular patient, such as heavy smoking, bruxism, or a lack of bone support.
“Treat any periodontal or peri-implant pathosis in the mouth before implant replacement.”
These situations require greater caution and additional action before moving forward with reimplantation. The authors recommended allergy or immunologic testing, bacterial culturing, bone quality and occlusion evaluations, and improving the patient's oral hygiene if necessary.
When and why a patient's implant failed are highly relevant and also lead to therapeutic considerations.
"The decision to treat or extract a compromised, nonmobile implant is difficult, because selecting a degree of osseous resorption surrounding a fixture that defines it as 'hopeless' is problematic," the authors explained. Some studies stated that a nonmobile implant with 50% bone loss meant that it had failed; however, these authors feel that this is too low.
"We suggest that a fixture should be characterized as doomed when 75% of the supporting bone has been resorbed, or there is less than 3 mm of apical bone around the implant and there are signs of inflammation," they wrote.
One of the primary takeaway messages from their analysis is a set of recommendations for clinicians once they have determined with certainty that an implant is failing. Despite the increased risk of failure relative to the initial implant placement, the potential benefits of a successful reimplantation are "profound," the study authors noted. In their opinion, an attempt is worthwhile. Of course, the patient should be fully informed and involved with making the decision to replace the implant or not.
To minimize risk, they noted the following:
- The clinician should treat any periodontal or peri-implant pathosis in the mouth before implant replacement.
- Ensure there is adequate bone height and width to maintain an implant or that the bone is augmented to provide appropriate support.
- Select suitable implants.
- Avoid contamination during surgical procedures.
- Do not overheat the bone.
- Construct a proper implant prosthesis.
- Instruct patients regarding good oral hygiene.
- Emphasize and provide maintenance care and overengineer cases in which the patients have parafunctional habits.