When creating a treatment plan for impacted maxillary canines, conventional radiographs will likely work fine for most cases. But if a case is particularly difficult to diagnose in the initial evaluation, a cone-beam CT (CBCT) scan may be the better option, according to a new systematic review.
Because CBCT scans are more expensive than traditional radiographs and expose patients to additional radiation, researchers from the Loma Linda School of Dentistry and Harvard School of Dental Medicine wanted to see if the benefits of 3D images outweighed the drawbacks. After examining the scientific literature, they concluded that CBCT should not be clinicians' first choice for imaging these cases.
"CBCT may be indicated for localizing the assessment of an impacted tooth when the information cannot be obtained adequately by lower-dose conventional radiography," wrote the study authors, led by Ehsan Eslami, DDS, from the Loma Linda School of Dentistry (American Journal of Orthodontics and Dentofacial Orthopedics, February 2017, Vol. 151:2, pp. 248-258).
Should you use CBCT or traditional x-rays?
After third molars, maxillary canines are the most commonly impacted teeth, which can lead to functional and aesthetic problems, according to Dr. Eslami and colleagues. Orthodontists and other clinicians have traditionally used 2D images to create treatment plans for those with impacted teeth, but traditional radiographs may have relatively poor visibility and distortion.
While CBCT addresses these drawbacks, the 3D scans also cost more and expose patients to higher levels of radiation. The researchers, therefore, reviewed the scientific literature to see if one type of image was better for treatment planning and accurately determining the location of impacted maxillary canines.
After searching through several online and offline tools, Dr. Eslami and colleagues ended up with eight studies, published between 2006 and 2014, that looked at radiographs versus CBCT images for impacted maxillary canines. The majority of the studies were cross-sectional observational studies, but two evaluated diagnostic accuracy.
CBCT was more accurate than conventional radiography, according to the review. CBCT images also tended to be more reliable, offering a more precise location of the impacted teeth and other dentine structures.
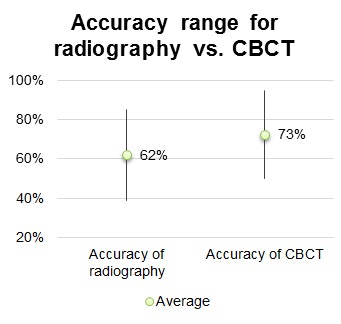
While the CBCT scans appeared to outperform traditional x-rays, the authors cautioned that it is too soon to say one technology is definitively better than the other. Although the scans may be useful when conventional radiographs cannot provide enough information about a tooth and surrounding structures, they also may not be appropriate for all cases.
"There is no robust evidence to support using CBCT as a first-line imaging method for impacted maxillary canine evaluation, but it is indicated when conventional radiography does not provide sufficient information," the authors concluded. "However, there is still a lack of evidence in relation to patient outcome efficacy and societal efficacy in the decision-making process."
What research is still needed?
Dr. Eslami and colleagues cautioned the eight studies they used had a high risk of bias, most often for not including randomized patient populations. In addition, the results of the included studies may be skewed by who was reading and analyzing the images, since radiologists tend to use traditional radiographs more effectively than orthodontists.
The study authors also hypothesized that CBCT may be better for complex cases involving impacted maxillary canines, but they noted that no studies have compared CBCT and radiography in cases with varying complexity levels. They hope future studies look at case difficulty and also investigate the societal and economic aspects of CBCT versus radiography.
"Although the importance of the diagnostic and therapeutic efficacy for a given medical imagining is evident, it is also needed to develop an appreciation of the connection between costs and achieved benefits," the authors wrote. "A part of this priority is the quantification of cost-effectiveness, cost-utility, and cost-benefit analysis."