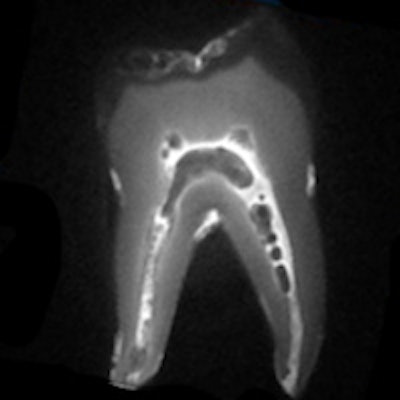
A growing body of research has demonstrated the potential for magnetic resonance imaging (MRI) in clinical dentistry, including endodontics, prosthodontics, and orthodontics.
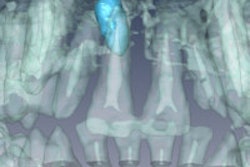
But there has been little analysis of how dental materials in a patient's mouth may affect the end result, according to a new study in Dentomaxillofacial Radiology (June 2013, Vol. 42:6).
"Magnetic susceptibility information is not readily available for many materials used in dentistry, especially those containing several components," wrote the study authors, from the University of California, San Francisco; University of Würzburg; and University of Regensburg. "Partly contradictory results have been reported regarding the severity of image artifacts caused by different dental materials."
Such artifacts are most likely caused by one of two things: eddy currents induced by alternating gradients and radiofrequency magnetic fields, and distortion of the static magnetic field due to the difference in magnetic susceptibilities of materials and body issues, the researchers noted.
Degree of compatibility
Using a 1.5-tesla MRI system (Magnetom Avanto, Siemens) and spin-echo and gradient-echo pulse sequences, the researchers investigated the potential influence of metal, ceramic, polymer, and composite dental materials on MRI. They then applied the geometric method to determine the magnetic susceptibility of the materials, and classified the materials based upon their degree of compatibility with MRI.
"Although the magnetic susceptibility values of many materials are unavailable, they can be estimated from the caused distortions in an MR image," they wrote.
Here is a list of the materials included in the study:
- AH Plus resin (Dentsply)
- Amalgam (Degussa)
- Cobalt chrome (CoCr; Amann Girrbach)
- Composites: Filtek Supreme XT Universal, Filtek Supreme XT Flowable, Filtek Z250, Filtek P60 posterior restorative (all 3M ESPE); Tetric Ceram, Tetric Flow (Ivoclar Vivadent)
- Glass ionomer cementer (3M ESPE)
- Gold alloy (DeguDent)
- Gold-ceramic crown (DeguDent)
- Gutta-percha (Demedi-Dent)
- Titanium alloy (Friadent)
- Zirconium dioxide (Metoxit)
- Orthodontic wires: Nickel-titanium (NiTi) alloy wire, stainless steel wire, stainless steel brackets (all Dentaurum)
"The tested materials showed a range of distortion degrees," the study authors wrote.
Even so, several were classified as fully compatible, meaning they can be present during an MRI exam even in the tooth of interest, and even if a very precise reconstruction of the tooth surface is required: AH Plus resin-based sealer, glass ionomer cement, gutta-percha, zirconium dioxide, and some composites.
Iron oxide pigments
While none of the 3M ESPE composites studied caused any detectable distortions, all of the Ivoclar Vivadent composites in the study caused "significant" artifacts, the researchers noted.
"Whereas composites of some manufacturers had an almost perfect susceptibility match to water and were therefore compatible for dental MRI, other showed markedly paramagnetic properties and caused significant distortions," they wrote.
This could be because manufacturers of these products often use iron oxide pigments, and "the smallest contamination by ferromagnetic substances can drastically alter the susceptibility of a magnetically compatible material," they noted.
In addition to the Ivoclar Vivadent composites, amalgam, gold alloy, gold-ceramic crowns, titanium allow, and NiTi orthodontic wires were classified as compatible I, meaning the material produces "noticeable distortions" and that acceptance when undergoing MRI depends on the application.
The stainless steel orthodontic appliances and the CoCr sample showed the strongest distortions and were classified as noncompatible, meaning these materials produce strong image distortions even when located far from the imaging region, according to the study authors.
"Although solutions for artifact correction are being sought, foreign materials in the body remain an issue," they wrote.
Their proposed compatibility classification system, which is based on quantifiable magnetic susceptibility, could serve as a guideline for future MRI research in dentistry, they concluded.
MRI's future in dentistry
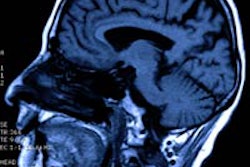
Totally noninvasive MRI applied to brain, maxillofacial, and even dental imaging shows a high sensitivity and specificity for many diseases, noted Djaudat Idiyatullin, PhD, who is involved in dental MRI research and development at the University of Minnesota Center for Magnetic Resonance Research.
"MRI certainly has a future [in this field], and it is unfair that in the future somebody having some paramagnetic filling in his mouth would be denied the advantages of MRI screening," he told DrBicuspid.com. "That is why I think this study analyzing this problem is very important to somehow stimulate the manufacturers to develop new materials with matched magnetic susceptibility, and also to help dentists avoid using MRI noncompatible materials in the practice."
It would be good to have some regulatory standards requiring the magnetic susceptibility value limit for such materials, he added.
Julian Boldt, PhD, of the University of Würzburg and co-author on the Dentomaxillofacial Radiology study, agreed.
"The materials we tested are commercially available, but there are commercially available alternatives that are MRI compatible," he told DrBicuspid.com. "Other materials will have to go the same way if MRI gets off the ground in dentistry, which I think it will."
Boldt and his colleagues are close to completing a prototype of a dedicated dental MRI scanner and are looking for commercialization partners. In addition to diagnostic imaging, MRI has also shown potential for therapeutic applications in dentistry, such as digital impressioning, he noted.