Just as the dental community is starting to get comfortable with cone-beam CT -- and becoming more aware of the ionizing radiation risks it poses if not used properly -- another well-established diagnostic technology appears headed for the dental operatory: magnetic resonance imaging (MRI).
Two presentations to be given at the International Association for Dental Research (IADR) conference next month in San Diego will showcase novel MRI technology developed at the University of Minnesota that is being tailored for use in both soft- and hard-tissue dental imaging applications.
While conventional MRI offers many diagnostic advantages, including the fact that it does not utilize ionizing radiation and can image soft-tissue structures with great precision and detail, it also has some challenges. The equipment can be claustrophobic to many patients, the imaging process is extremely loud and typically takes 30 to 60 minutes, and it requires several expensive and sensitive components; in particular, MRI requires high-power radiofrequency amplifiers to attain a sufficiently intense radiofrequency field.
|
How magnetic resonance imaging works Magnetic resonance imaging (MRI) generates cross-sectional images of the human body by using principles of nuclear magnetic resonance. MRI uses a powerful magnetic field to align the nuclei within the atoms of the patient's body. Radiofrequency pulses are then applied, prompting the nuclei to release some of the radiofrequency energy. The energy that is absorbed by different atoms in the body is echoed or reflected back out of the body. These echoes are continuously measured by the MR scanner, and a digital computer reconstructs these echoes into images of the body. A computer then produces detailed pictures of tissues and body structures. The loud tapping heard during an MRI exam is created when the gradient coils are switched on and off to measure the MR signal reflecting back out of the patient's body. |
These issues prompted Michael Garwood, PhD, and colleagues in the Center for Magnetic Resonance Research (CMRR) at the University of Minnesota, to develop SWIFT (sweep imaging with Fourier transformation). Unlike conventional MRI methods with large pulsed radiofrequency signals and signal detection from echoes, SWIFT is a fast, quiet MRI method that uses frequency-swept radiofrequency signals with almost instantaneous signal acquisition. In addition, SWIFT is more tolerant to static magnetic field inhomogeneity, according to its developers, and its short acquisition delay makes it relatively insensitive to motion.
The main advantage of SWIFT is its nearly simultaneous excitation and acquisition scheme (Journal of Magnetic Resonance, August 2006, Vol. 181:2, pp. 342-349). In conventional MRI, excitation and acquisition events are separated by echo time -- typically more than 1 millisecond. This creates some imaging limitations, according to Djaudat Idiyatullin, PhD, an assistant professor at the CCMR and co-inventor of SWIFT.
"When you have this delay, you have a fast decaying signal you cannot detect," he said. "When water molecules are highly restricted in motion, like in the hard dental tissue, the MR signal it gives off is very fast and traditional MRI cannot see it because it waits too long before it acquires the signal."
But with SWIFT, the signal acquisition can begin within a few microseconds after excitation, so it can see things that can't be seen with traditional MRI, he added.
"All modern MRI is based on sequential flight," Idiyatullin said. "Excitation is separate in time from acquisition, and only one sequence is measured during signal excitation. But it is much easier to do MRI when separating acquisition from excitation, and SWIFT was born only when we figured out how to extract object information from the measurements during excitation."
It also reduces the noise typically associated with MRIs because the gradient is always on and adjusted only in small increments throughout the scan, according to Don Nixdorf, DDS, an assistant professor at the University of Minnesota School of Dentistry. Idiyatullin and Dr. Nixdorf are both consultants for Steady State Imaging (SSI), a Minnesota company founded by Garwood -- an associate director of the CMRR -- to commercialize SWIFT for medical and industrial applications.
"Conventional MRI is very loud -- up to 90 decibels -- due to the gradient coils rapidly changing the magnetic field in and around the object so it can separate them," Dr. Nixdorf said. "SWIFT doesn't do that, so it is very quiet." It accomplishes this by using a small step when changing gradients between projections, thereby avoiding the fast gradient switching that creates the loud tapping noise associated with conventional MRI.
10 years out
In beta testing at the Vanderbilt University Institute of Imaging Science and the University of Texas Southwestern Medical Center, SSI has been focused on preclinical animal imaging applications. But the company is also beginning to investigate clinical applications in oncology, breast imaging, neurology, cardiology, and dentistry.
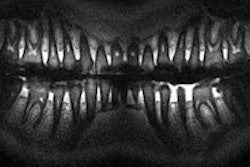
"The biggest advantage for dentistry is that SWIFT can simultaneously see hard and soft tissue," Dr. Nixdorf said. "You can see inside the tooth, the tooth pulp, and you don't have to look for bone loss because you can see the water content right away."
 SWIFT, a novel MRI technique, can simultaneously image both hard and soft dental tissue. Image courtesy of Djaudat Idiyatullin, Curt Corum, and Steen Moeller (CMRR).
SWIFT, a novel MRI technique, can simultaneously image both hard and soft dental tissue. Image courtesy of Djaudat Idiyatullin, Curt Corum, and Steen Moeller (CMRR).
At the IADR meeting, Dr. Nixdorf and Idiyatullin will each give a presentation describing some of the work they have been doing in this field.
Idiyatullin will provide an overview of SWIFT and its potential applications in clinical dentistry, describing in vivo SWIFT experiments performed at the University of Minnesota. In these experiments, the researchers found that SWIFT MRI offered simultaneous visualization of densely mineralized tissues (enamel and dentin) and soft tissues in the pulp, within clinically relevant scanning times (less than 10 minutes) and without the use of ionizing radiation.
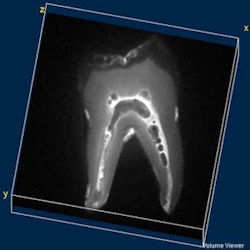
In his presentation, Dr. Nixdorf will describe a small study conducted at the University of Minnesota that compared SWIFT with microCT for early caries detection. Fifteen early carious lesions were placed in 15 tooth samples with remineralization attempted in 10. All samples were stored in isotopic saline and imaged after being patted dry. MRI was performed using a 9.4-tesla Varian Medical Systems unit with DirectDrive and a custom-fabricated radiofrequency coil. The reference standard was microCT.
Calculations of sensitivity and specificity were used to determine diagnostic accuracy. Both sensitivity and specificity of the MRI system was 80%, according to the researchers. Given the enhanced contrast MRI has over x-ray-based techniques, since the relative change of water content is greater than mineral content in densely calcified tissues, research assessing in vivo use is warranted to explore potential for develop for clinical applications, according to Dr. Nixdorf.
And what about the negative effects that metal-based materials can have on MRI images?
"As it stands now, the restorative materials that are nonmetallic do not pose a problem, while others -- such as amalgam -- only impose small amounts of distortion (less than with cone-beam CT) because the signal accession using SWIFT occurs so quickly the individual protons do not have time to to become distorted," he said. "Furthermore, the development of mathematical algorithms, which effectively remove the distortion imparted by metallic objects, is an active area of research at the University of Minnesota and other places since the presence of such objects is problematic for imaging all parts of the human body. Since this distortion is greatly reduced with SWIFT, the application of such algorithms is more fruitful."
Dr. Nixdorf is not alone in his belief that MRI will become a clinical tool for dentistry in the not-too-distant future. During a panel session at the American Academy of Oral and Maxillofacial Radiology annual meeting last November, Kristine Mosier, DMD, PhD, an associate professor of radiology at the Indiana University School of Medicine, said she expects to see MRI in dental offices within the next 10 years.
"With the way MR technology is evolving, we will begin to see smaller, less expensive systems for intraoffice and even intraoral use," she said.