
Dental practitioners have long relied on articulating paper to determine occlusal contact. But some occlusion experts believe there is a better approach, especially when it comes to analyzing bite force and timing.
"Articulating paper is used to mark the teeth to be able to find the right spot and study the bite and assess the bite forces by looking at the ink marks and interpreting them based on size," said Robert Kerstein, D.M.D., a former assistant clinical professor at Tufts University School of Dental Medicine who specializes in prosthodontics and occlusion at his Boston-based practice. "Big marks mean lots of force, little marks mean less force. This is what has been taught in all the textbooks and dental schools for years."
But this is the opposite of the physical truth, he claims. In fact, the problem with articulating paper is that it does not describe occlusal forces or accurately measure the bite force in any quantifiable and predictable way, said Dr. Kerstein, who is also a clinical consultant for Tekscan, which manufactures the T-Scan III computerized occlusal analysis system.
"The dental public is being shortchanged because they spend thousands of out-of-pocket dollars on aesthetic, implant, and complex prosthodontic treatment plans, only to have their dentist, at the end of treatment, use the articulating paper mark size as their guide to adjust the bite," he told DrBicuspid.com. "The dentists and the public both truly deserve to know there is an alternative to this subjective guessing available to them."
In an analysis of 600 paper markings made at varying human occlusal loads on epoxy dental casts, Dr. Kerstein and colleagues from the University of Alberta determined that articulating paper mark size can vary so greatly at a given human occlusal load that an operator would be unable to determine from visually inspecting the marking which marks were forceful and which were not (Open Dentistry Journal, 2007, Vol. 1, pp. 1-7). Only 21% of the marks correlated to the applied occlusal load, while 79% of the marks did not describe the applied load that imprinted the marks to the casts, the authors reported.
"What this means to the clinician is that choosing the marks to adjust based on their size is highly error-prone," Dr. Kerstein told DrBicuspid.com. "Computer analysis makes it possible to accurately measure occlusal forces in a predictable, nonsubjective way. And this computer-based method has been shown over the past 25 years to have numerous health advantages for dental patients everywhere."
Adjunct, not replacement
Other occlusal experts believe the T-Scan system is most useful as an adjunct to articulating paper, particularly when treating more occlusally challenging conditions, such as temporomandibular disorder.
"For some reason, the company [Tekscan] has taken the stance that the best way to market and sell this product is to convince dentists that articulating paper is worthless and that what they've been doing all these years is wrong," said John Cranham, D.D.S., clinical director of the Dawson Academy. "The company should emphasize that this tool is something that will allow them to do some things better."
Tekscan does not see the T-Scan as a replacement for articulating paper but as an interpretive tool, according to Brent Thompson, sales and marketing manager for the company.
"You still need articulating paper [with the T-Scan], but the paper is just for marking the teeth to see where they hit. T-Scan measures the timing and time sequencing of the contacts," he said. "So dentists can use the T-Scan to interpret what the marks are showing them."
Dr. Cranham, who uses the T-Scan regularly in his practice but has no affiliation with the company, agrees.
"When looking at [articulating paper] dots on teeth, you are looking at the sum totality of time, so you don't always know which teeth are hitting first," he said. "But with T-Scan, you can go all the way back to when teeth are first occluding and see which are hitting first. The T-Scan creates a dynamic movie that allows us to look at contacts on teeth in 1/100th of a second increments. It records the sum of the time it takes for the teeth to occlude and disocclude."
 |
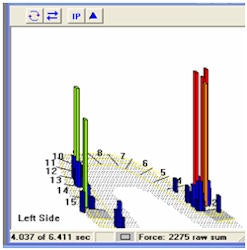
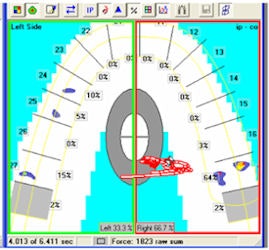
| Above, you see at points A and B a very scratchy small mark that dentists are taught to interpret as "light force." Below left (A) and right (B), the computer shows it to be very, very forceful. A dentist will leave this high force area alone and not treat this damaging contact because the paper mark appears "light." All images courtesy of Robert Kerstein, D.M.D. |
  |
"For a long time we were dealing with materials such as gold or silver that were more malleable, so if the occlusion was off, there was a better chance that it would settle into its own," he said. "But now we are using so many bonded glass materials, and the first sign of instability with ceramic is often fracture. So although the T-Scan adds time during the initial restorative appointment, it saves a lot of time in later adjustments and fractures."
Controlled trials needed
|
How the T-Scan works The technology behind T-Scan was originally developed in 1984 by William Maness, D.D.S., M.S., at Tufts University (he is no longer affiliated with the company) and introduced commercially in the late 1980s by Tekscan. The system has since gone through several iterations as the supporting technologies have evolved. The current version, T-Scan III, features a paper-thin, arch-shaped, pressure-sensitive sensor made of mylar that is connected to a Windows-based computer via a USB port.
When the patient bites down on the sensor pad, the pad measures the specific amount of force on the occlusal surface of every tooth and the timing of the forces. The resulting information is displayed in real-time as a dynamic "bite force movie" that illustrates the various occlusal pressures with colors during playback. The darker colors represent low occlusal pressure, while the brighter colors indicate higher occlusal pressures. |
However, these features come at what some -- including Dr. Cranham -- consider to be a high cost, literally.
"I definitely think this is an extremely good tool, but the price," Dr. Cranham said. "If it was $2,000 to $3,000, they would have better market penetration, but for $10,000. ..."
Even so, he would not practice without it, he said. "Dentists have a hard time justifying the cost of this technology until they use it," he noted. "Then and only then does it become extremely valuable."
Others cite the lack of long-term, objective, controlled studies of the T-Scan. While several papers on the technology and its applications have been published, the majority include Dr. Kerstein as a co-author. However, this is changing, with more independent research projects beginning in Germany, France, England, Turkey, and Poland, according to Thompson.
In fact, he believes that as the technology evolves and clinicians become more familiar with its capabilities, new applications will continue to open up, which will in turn lead to advances in research.
"I think the T-Scan is going to bring a lot more understanding to occlusion in general," Thompson said. "People talk about the forces on teeth, and we can measure force distribution from the left to the right side. We also have the ability per tooth to identify the amount of force for each one. There is no research out there that we are aware of that even tells what the percentage of force should actually be per tooth. I think the T-Scan will help promote this kind of research."
For Dr. Kerstein, who began using the T-Scan in 1984 when it was first built and continues to use it today, the choice is simple.
"The core issue [with articulating paper] is that the dentist is guessing at the end result, which is a bad medical standard," he said. "Why should we be treating patients poorly when there is this amazing technology out there?"
Copyright © 2009 DrBicuspid.com
















