Research has long shown that women are at increased risk for oral health problems -- notably periodontitis and alveolar bone loss -- compared to men due to physiological changes associated with hormonal fluctuations that occur from puberty through menopause.
Now a new literature review concludes that postmenopausal women are even more susceptible to periodontal disease and related conditions, according to researchers from the Cleveland Clinic and Case Western Reserve University School of Dental Medicine (Cleveland Clinic Journal of Medicine, August 2009, Vol. 76:8, pp. 467-475).
“The cytokines are telling us we need
to talk.”
— Leena Palomo, D.D.S., M.S.D.,
Case Western Reserve University
School of Dental Medicine
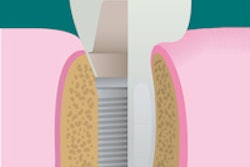
The rate of whole-body bone loss in postmenopausal women is a predictor for tooth loss, noted Leena Palomo, D.D.S., M.S.D., director of predoctoral periodontics at Case Western, and her colleagues in the journal article. Based on a 1996 study on the relationship between tooth loss and bone loss, "for every 1% per year decrease in whole-body bone mineral density, the risk of tooth loss increases more than four times" (Calcified Tissue International, December 1996, Vol. 59:6, pp. 433-437). Another study found that women with severe osteoporosis were three times more likely than healthy, age-matched controls to be edentulous (Journal of Prosthetic Dentistry, February 1990; 63:2, pp. 218-222).
"We know that the population is aging and that women are missing more teeth than men even though they go to the dentist more and report better oral hygiene rates," Dr. Palomo said. "So we wondered what the problem is."
One culprit may be estrogen deficiency, which can lead to alveolar bone loss in the presence of bacterial biofilm and ultimately periodontitis, if left untreated, she said.
"The key thing about menopause is that the estrogen-deficient host is related to cytokines, which are part of the bone resorption cascade," Dr. Palomo said. "When activated in the presence of bacterial biofilm and left untreated, it may in turn lead to severe periodontitis."
The notion that estrogen deficiency is a risk factor for periodontal disease was first proposed more than a decade ago, she and her colleagues noted in their article, pointing to a model developed by Robert Genco, D.D.S., Ph.D., and Sara Grossi, D.D.S., M.S. (Compendium of Continuing Education in Dentistry Supplement, 1998, Vol. 22, pp. S23-S29).
"In this model, estrogen deficiency leads to more production of bone-resorbing cytokines produced by immune cells and osteoblasts," Dr. Palomo and colleagues wrote. "When challenged by products related to periodontal bacterial plaque biofilm, by bone-resorbing factors such as lipopolysaccharides, and by toxins, the host immune system produces more inflammatory cytokines that activate osteoclasts, which reabsorb bone. The buildup of bacterial plaque biofilm made up of periopathogenic bacteria seems to be necessary for an estrogen-deficient woman to actually show changes such as loss of tooth attachment and alveolar bone."
In fact, bacterial biofilms also play a key role in postmenopausal periodontal destruction, Dr. Palomo added. The solution is simple: Postmenopausal women should be strongly encouraged to maintain good oral hygiene by their caregivers.
Bisphosphonates and ONJ
Dr. Palomo and her colleagues also looked at the relationship between bisphosphonate use and osteonecrosis of the jaw (ONJ). They cited studies indicating the positive effect bisphosphonates can have on systemic bone resorption and bone fractures, including studies focused specifically on the jaw.
For example, in a cross-sectional study by Dr. Palomo and other groups, postmenopausal women with low bone density using risedronate for at least three months showed significantly less plaque accumulation, less gingival inflammation, lower probing depth measurements, less periodontal attachment loss, and greater alveolar bone levels (Menopause, November/December 2005, Vol. 12:6, pp. 685-690). And a double-blind controlled prospective trial found that six months of alendronate therapy significantly improved periodontal disease in 40 postmenopausal women with established periodontal disease (Journal of Periodontology, December 2004, Vol. 75:12, pp.1579-1585).
These and related studies cited in their article led Dr. Palomo and her colleagues to determine that "To date, no cause and effect relationship between osteonecrosis of the jaw and bisphosphonate use has been established. Further studies are needed to fully explore this relationship." Dr. Palomo's group is, in fact, currently exploring novel periodontal assessments comparing the oral health of postmenopausal women with osteoporosis who are not on bone therapy with postmenopausal women with osteoporosis treated with bisphosphonates for two or more years.
In the mean time, "regardless of whether the patient is receiving a bisphosphonate drug, physicians caring for postmenopausal women should be vigilant and encourage their patients to seek regular dental evaluation for prevention and early management of oral disorders," Dr. Palomo and her colleagues concluded.
"The basic point is that physicians who are dealing with menopause care need to communicate with the dentists so that these women can get all the types of care they need," Dr. Palomo said. "The cytokines are telling us we need to talk."
Copyright © 2009 DrBicuspid.com