Imaging helped clinicians diagnose and treat rare orbital and mouth abscesses caused by a dental infection in a 13-year-old boy, according to a case report recently published in the European Journal of Dentistry. If untreated, the condition could have led to death or blindness.
The boy's main symptom was two days of dental pain, which progressed to his periorbital tissues, and he began experiencing vision problems. A computed tomography (CT) scan allowed clinicians to quickly diagnose and manage his condition, the authors wrote.
"Multidisciplinary and timely management is crucial for successful outcomes in managing orbital abscesses of odontogenic origin," wrote the group, led by Dr. Ashley Houle of the University of Illinois at Chicago (Eur J Dent, August 13, 2021).
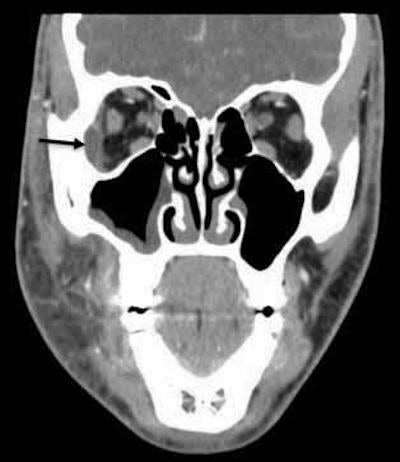 A CT scan (coronal section) shows the patient's right lateral orbit subperiosteal abscess, identified by a black arrow, and right maxillary sinusitis. All images courtesy of Houle et al. Licensed under CC BY 4.0.
A CT scan (coronal section) shows the patient's right lateral orbit subperiosteal abscess, identified by a black arrow, and right maxillary sinusitis. All images courtesy of Houle et al. Licensed under CC BY 4.0.It is rare for an odontogenic infection to cause an orbital abscess, but when it does it can have severe effects, including a cavernous sinus thrombosis that can lead to death. Timely recognition and management of this condition can prevent serious complications.
After a two-day history of persistent right maxillary dental pain with associated swelling, the 13-year-old boy was taken to the emergency department. He had recently undergone a routine dental evaluation and cleaning, and excavation and restoration of dental caries was planned within the month, according to the authors.
The boy was given 900 mg of clindamycin intravenously at the outside hospital, and he was transferred the same day to the University of Illinois Medical Center for specialty evaluation.
When he arrived at the medical center, his right eye was swollen shut. His vision was blurry when he manually opened his eyelids. Also, he felt pain on the right side of his face when he moved his eye.
A clinical exam found that the boy had severe right periorbital and midface edema, as well as mild emphysema of the right upper eyelid. An eye exam showed 20/20 vision with no optic nerve problems, mild restriction to adduction, and slightly elevated intraocular pressure. Intraorally, tooth #3 had a large restoration with adjacent fluctuant vestibular swelling but no active drainage.
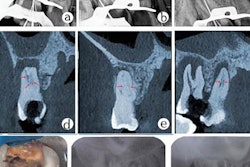
 A panoramic radiograph shows the restoration of tooth #3 with periapical radiolucency and right maxillary sinusitis.
A panoramic radiograph shows the restoration of tooth #3 with periapical radiolucency and right maxillary sinusitis.In addition, a CT scan taken at the outside hospital was reviewed by medical center clinicians. They identified a subperiosteal abscess at the right lateral orbit. The right canine space abscess came from the buccal roots of tooth #3. Also, the scan showed that fluid collected at the right canine space superiorly and posteriorly to the right lateral orbit, and right maxillary sinusitis was present.
To treat the boy, clinicians decided to place him under general anesthesia to drain the abscesses surgically and extract tooth #3. Specimens taken from the right orbital tissue were positive for Peptostreptococcus micros and Prevotella denticola. Samples taken from the right canine space were positive for Haemophilus parainfluenzae, Rothia mucilaginosa, and Streptococcus mitis/oralis, according to the authors.
While admitted to the medical center, the boy was given 3,000 mg of intravenous ampicillin-sulbactam every six hours and told to swish with 15 mL of 0.12% chlorhexidine gluconate solution twice per day. Also, 0.5% erythromycin ophthalmic ointment was applied to the right eyelid four times per day.
After discharge, the patient continued taking antibiotics and using the mouth rinse and eye cream. He experienced no further complications and his vision improved, the authors wrote.
Pediatric patients who present at emergency departments and dental offices often complain of dental pain. Clinicians should escalate care when pain is coupled with periorbital edema and visual changes, they wrote.
"It is crucial for emergency and primary care physicians to recognize when specialist consultation is indicated and expedite this process," Houle and colleagues concluded.