A 16-year-old girl developed Nicolau syndrome, a rare complication following an intramuscular injection, during a root canal, causing necrosis and leaving her with lasting scars on most of her face. The case report was published on February 20 in the Journal of Endodontics.
This latest report is the seventh reported case of an adverse reaction to an intramuscular injection of calcium hydroxide. In 2000, the first clinical case report of this condition involving a 27-year-old man in Belgium was published, the authors wrote.
“To minimize the risk of NS (Nicolau syndrome), dentists should exercise caution by avoiding forced injection of CH (calcium hydroxide) during treatment, particularly when the root canal is actively bleeding,” wrote the authors, led by Dr. Wentao Qian of the department of oral surgery, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine in China.
A 16-year-old girl with swelling, pain
The girl went to the hospital after having swelling and pain on the right side of her face for a week. She had a pulp polyp on the surface of tooth #30 and had a root canal in the lower right posterior tooth while under local anesthesia.
During the pulp extirpation, the dentist encountered bleeding in the canal and then applied calcium hydroxide. Suddenly, the teen experienced a headache accompanied by nausea and vomiting. For about 10 seconds, the girl was unconscious. When she regained consciousness, her headache had not improved, and her face and lips turned blue, they wrote.
She was sent to the emergency department and underwent magnetic resonance imaging. The suspected diagnosis was cavernous sinus syndrome, and the girl was prescribed anti-inflammatory treatment.
The next day, the patient was transferred to another hospital and underwent a lumbar puncture exam to rule out the possibility of an intracranial infection. After receiving anti-inflammatory and neurotrophic treatment for one week, the patient's facial cyanosis became more severe, the authors wrote.
The girl had ecchymosis on the side of her face, skin necrosis on the right nostril and nasal tip, swelling and cyanosis of the upper lip. Additionally, there was erosion and necrosis of the mucosa of the hard palate, buccal mucosa, and oral commissure. She was having significant pain opening her mouth. She had a lack of sensation, and she had erosion in the buccal gingival region of tooth #30.
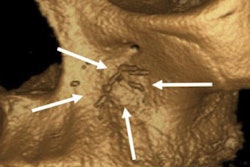
A panoramic x-ray revealed a radiolucency in the facial and inferior alveolar arteries, and computed tomography scans highlighted high-density areas in the facial, inferior alveolar, and infraorbital arteries. Based on a thorough analysis of her medical history, clinical symptoms, and imaging findings, the girl was diagnosed with Nicolau syndrome, the authors wrote.
A digital subtraction angiography exam pinpointed the exact location of the embolism. The exam revealed occlusion in the distal segments of the right maxillary and facial arteries that were blocking the blood supply to the patient’s cheek and nasal regions, they wrote.
Due to a time lapse of more than a week, a multidisciplinary team, including vascular surgeons and neurosurgeons, concluded that revascularization interventions would likely not be successful. Therefore, a conservative management approach, which included anti-inflammatory, analgesic, and neurotrophic drugs, as well as psychosocial support, was taken, the authors wrote.
After 10 months, the teen’s necrotic facial tissue began to shed, resulting in a tissue defect in the right nasal alar crease. Also, she developed extensive scarring, leading her lower eyelid to become everted, they wrote.
A challenging syndrome
Nicolau syndrome, which is characterized by severe injection site pain and the development of a purplish discoloration, has no definitive treatment plan, and the pathogenesis is unknown, according to the report.
When Nicolau syndrome occurs subsequent to endodontic treatment, it commonly manifests in the molar area and is not limited by gender, age, or race. A similarity among all reported cases was that dentists encountered bleeding within root canals during treatment and proceeded to directly inject calcium hydroxide without fully stopping bleeding. Typically, patients feel immediate face pain and numbness after the injection, and the maxillofacial skin whitens on the same day that eventually progresses to facial tissue necrosis, the authors wrote.
Preventing Nicolau syndrome is the most effective strategy to treat it. Therefore, injectable calcium hydroxide should be avoided during root canal bleeding, they wrote.
“In the event of NS, early initiation of thrombolytic and anticoagulant therapy is crucial to minimize the occurrence and severity of ischemic necrosis,” Qian and colleagues wrote.