A 71-year-old man ingested a nearly 2-inch piece of dental material that ended up stuck in the lower part of his throat while having impressions taken at a Kentucky clinic. The clinical report was published in the Journal of Prosthetic Dentistry.
Clinicians could not detect the lodged impression material radiologically, so an otolaryngologist planned to remove the object surgically. But while preparing for the procedure, the man bent down to untie his shoes and coughed, which removed the stuck material.
Though the man avoided surgery, this case highlights the importance of taking special care when performing impressions on patients, the authors wrote. This is especially true for older patients and those with dysphagia and weakened gag reflexes.
"Given the potential for morbidity and mortality that may arise from such misadventures, all dental practitioners should implement preventive strategies to reduce the incidence of such events," wrote the authors, led by Dr. Fonda Robinson from the Ohio State University College of Dentistry (J Prosthet Dent, July 17, 2021).
From dental clinic to emergency room
The man visited the University of Kentucky College of Dentistry dental clinic to get impressions of his upper and lower teeth for the fabrication of removable dentures. In addition to having high blood pressure, the man experienced an occlusive cerebrovascular attack five years earlier that resulted in him experiencing some dysphagia, according to the report.
An operator adapted a green stick modeling plastic impression compound to the outside of a maxillary tray, then placed relief holes. Then, the operator followed the manufacturer's instructions to paint adhesive onto the tray surface and borders.
The tray was placed in the patient's mouth over his maxillary edentulous soft tissues, and the material was allowed to polymerize for about five minutes, the authors wrote. As the tray was being removed from his mouth, the patient gagged a little.
At that time, the operator saw a thin strand of polymerized impression material extending from the back of the tray, which looked like it had been separated or torn from additional material that could not be seen. The patient coughed several more times. He felt something at the base of his throat that he could not dislodge or swallow, but he could otherwise swallow and speak and showed no signs of respiratory distress.
Immediately, the man went to the emergency department, where an otolaryngologist saw the impression material in the man's hypopharynx. After several unsuccessful attempts by emergency department staff members to help him dislodge the material, the clinician ordered a lateral neck x-ray. The radiologists reported no significant radiographic findings, so the otolaryngologist planned to remove the object surgically, they wrote.
As the patient prepared for the operating room, he bent down to untie his shoes. He then forcibly coughed and dislodged the impression material on his own.
The otolaryngologist examined the man and confirmed that the material was no longer present in his hypopharynx. Fortunately, the man experienced no other related complications.
Prepare for everything
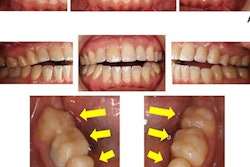
Upon examination, a prosthodontist determined the object in the patient's throat was consistent with polyvinyl siloxane impression material, according to the report. Based on the look of the recovered material, the object likely was stuck just dorsal to the trachea in the hypopharynx.
The material showed several anatomic parts, including the bilateral piriform recesses. The interarytenoid notch, which is a congenital variation of the larynx, could also be seen on the impression material, they wrote.
Cases like this one of aspiration or ingestion of foreign objects are well-documented risks in dentistry, the authors wrote. Clinicians and their teams must be prepared to manage these types of emergencies.
"The dental team must use risk reduction strategies by identifying and reducing risk factors whenever possible," Robinson and colleagues wrote.