Nonsurgical periodontal treatment may positively impact the lives of patients with diabetes, even when it does not directly improve diabetes indicators. The findings come from a new study investigating the effects of scaling and root planing on patients with type 2 diabetes.
The study is one of the first to look at quality-of-life factors for patients with type 2 diabetes who underwent nonsurgical periodontal treatment, according to the researchers. Their findings suggest that periodontal therapy may have hidden benefits for these patients.
"We reported that [quality-of-life] scores were improved following periodontal treatment," wrote the authors, led by Hirofumi Mizuno from the Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences in Okayama, Japan (PLOS One, November 16, 2017). "Treatment satisfaction influences compliance, which may contribute to the management of both diabetes and periodontitis."
Hidden benefits of periodontal treatment
Recent scientific reviews have called for researchers to quantify quality of life for patients with diabetes, yet few studies investigating the effects of periodontal treatment have included this outcome in their research. Therefore, the researchers of the current study were interested in whether nonsurgical periodontal therapy could improve quality of life for patients with type 2 diabetes. They also investigated the effect of scaling and root planing on oxidative stress levels and one frequently used diabetes indicator.
“Treatment satisfaction influences compliance, which may contribute to the management of both diabetes and periodontitis.”
The researchers began by recruiting 40 patients with type 2 diabetes and chronic periodontitis to participate in their six-month randomized clinical trial. All participants received supragingival plaque removal and oral hygiene instruction at the start of the study. They were then split into two groups: an intervention group that received nonsurgical periodontal treatment and a control group that did not.
The patients in the intervention group received at least 60 minutes of scaling and root planing from a general dentist. The periodontal treatment occurred during two or more sessions, and the sessions were completed within 42 days of the initial visit, as recommended by the Japanese Society of Periodontology.
All patients also completed a quality-of-life questionnaire. The questionnaire asked participants about diabetes' impact on their lives within the following four spheres:
- Burden on social activities and daily activities
- Anxiety and dissatisfaction with treatment
- Hypoglycemia
- Satisfaction with treatment
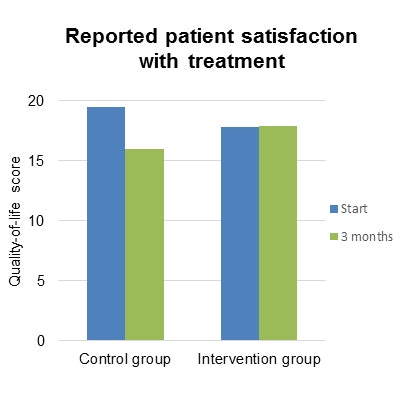
For the 28 patients who completed the full study, nonsurgical periodontal treatment did not significantly change hemoglobin A1c (HbA1c) levels, an indicator of how well diabetes is being controlled. However, even without changes to their HbA1c levels, patients who received periodontal treatment reported significantly higher satisfaction with their treatment than those who did not.
Nonsurgical periodontal treatment also significantly improved patients' oxidative stress levels, which is related to the development and progression of diabetes complications, the authors noted. For instance, improving oxidative stress may also improve glycemic control and reduce diabetes complications.
"Systemic oxidative stress affects the pathophysiology of diabetes ... [and] satisfaction with diabetes treatment contributes to compliance," the authors wrote. "Thus, periodontal treatment may be considered in patients with [type 2 diabetes] for its benefits of improving pathophysiology and compliance."
As expected, most periodontal markers improved for patients who received scaling and root planing. However, plaque control records did not significantly improve for the intervention group, which suggests that at-home oral hygiene and self-care may be a problem for these patients.
Long-term results still unknown
Previous studies have found that periodontal treatment can significantly improve hemoglobin A1c levels. The authors suggested their study design, which included patients who were already under a physician's care for diabetes and who had stable medication usage, may have impacted this finding in particular.
In addition, treatment satisfaction and oxidative stress levels were not significantly different between the control and intervention groups at six months, the authors noted. They suggested that future studies are needed to evaluate the long-term effects of these metrics.
"Further studies are needed to elucidate the factors involved in improving treatment compliance," they wrote. "In [type 2 diabetes] patients, nonsurgical periodontal treatment improved systemic oxidative stress balance and [quality of life], but did not decrease the levels of HbA1c as the main outcome at three-months follow-up."